Maniobras de movilización visceral en el trauma vascular abdominal
Resumen
Fundamento: el trauma vascular abdominal constituye un reto para el cirujano. El control vascular es una condición sine qua non en los pacientes que reciben intervención quirúrgica frente a esta letal enfermedad, donde las maniobras de movilización visceral constituyen una herramienta clave en el tratamiento.
Objetivo: explicar las maniobras de movilización visceral que pueden auxiliar al cirujano frente a un trauma vascular abdominal.
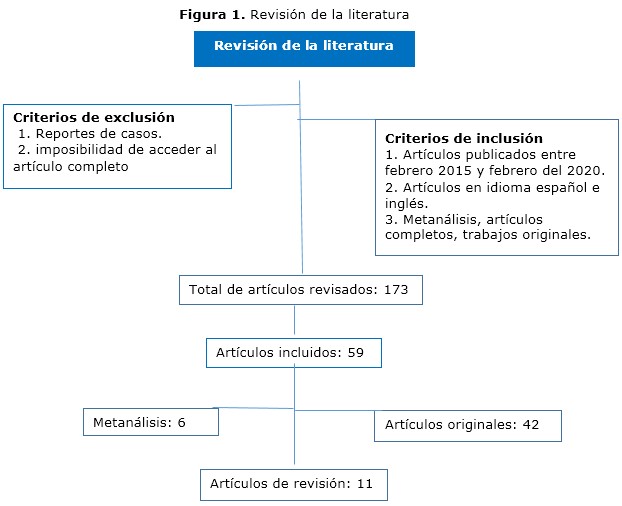
Métodos: se realizó una búsqueda en las bases de datos Scopus, Medline, Cochrane, Hinari y Redalyc se utilizaron los descriptores: trauma vascular, abdomen, maniobras, movilización visceral.
Resultados: se abordaron las maniobras de movilización visceral a tener en cuenta en el trauma vascular abdominal con una explicación de los principales pasos técnicos en cada una de ellas.
Conclusiones: el conocimiento y aplicación de las maniobras de movilización visceral constituyen una herramienta útil en el tratamiento de pacientes con trauma vascular abdominal.
DeCS: LESIONES DEL SISTEMA VASCULAR /cirugía; TRAUMATISMOS ABDOMINALES/complicaciones; VÍSCERAS/cirugía; PROCEDIMIENTOS QUIRÚRGICOS VASCULARES; PROCEDIMIENTOS QUIRÚRGICOS OPERATIVOS/métodos.
Referencias
Talbot E, Evans S, Hellenthal N, Monie D, Campbell P, Cooper S. Abdominal and Pelvic Vascular Injury: A National Trauma Data Bank Study. Am Surg [Internet]. 2019 [citado 18 Abr 2020];85(3):292-3. Disponible en: https://journals.sagepub.com/doi/10.1177/000313481908500335
doi.org/10.1177/000313481908500335
Warren KJ, Balogh ZJ. Major vascular trauma. Eur J Trauma Emerg Surg. 2019;45(6):941-2. doi: 10.1007/s00068-019-01267-2
Smith S, McAlister V, Parry N, Power A, Vogt K. Vascular trauma: Does experience in the United States apply to a Canadian centre? Can J Surg [Internet]. 2019 [citado 18 Abr 2020];62(6):499-501. Disponible en: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6877390/. doi: 10.1503/cjs.002317
D'Souza K, Bleszynski MS, Hawes HG. Rare constellation of abdominal vascular injuries in blunt trauma: Left gastric artery pseudoaneurysms and dissection. Int J Surg Case Rep [Internet]. 2019 [citado 18 Abr 2020];60:30-3. Disponible en: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6563334/.
doi: 10.1016/j.ijscr.2019.05.028
Avgerinos ED, Pikoulis E. Contemporary Strategies in the Management of Civilian Vascular Trauma. Front Surg [Internet]. 2018 [citado 18 Abr 2020];5:43. Disponible en: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6004396/.
doi: 10.3389/fsurg.2018.00043
Weale R, Kong V, Manchev V, Bekker W, Oosthuizen G, Brysiewicz P, et al. Management of intra-abdominal vascular injury in trauma laparotomy: a South African experience. Can J Surg [Internet]. 2018 [citado 18 Abr 2020];61(3):158-64. Disponible en: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5973903/.
doi: 10.1503/cjs.009717
Granite G, Pugh K, Chen H, Longinaker N, Garofalo E, Shackelford S, et al. Assessment of Anatomical Knowledge and Core Trauma Competency Vascular Skills. Mil Med [Internet]. 2018 [citado 18 Abr 2020];183(suppl 1):66-72. Disponible en: https://academic.oup.com/milmed/article-lookup/doi/10.1093/milmed/usx151 doi: 10.1093/milmed/usx151
Feliciano DV, Moore EE, Biffl WL. Western Trauma Association Critical Decisions in Trauma: Management of abdominal vascular trauma. J Trauma Acute Care Surg. 2015;79(6):1079-88. doi: 10.1097/TA.0000000000000869
Feliciano DV. Vascular Trauma Revisited. J Am Coll Surg [Internet]. 2018 [citado 18 Abr 2020];226(1):1-13. Disponible en: https://www.sciencedirect.com/science/article/abs/pii/S1072751517318422?via%3Dihub doi: 10.1016/j.jamcollsurg.2017.08.011
Pratschke S, Rauch A, Albertsmeier M, Rentsch M, Kirschneck M, Andrassy J, et al. Temporary Intraoperative Porto-Caval Shunts in Piggy-Back Liver Transplantation Reduce Intraoperative Blood Loss and Improve Postoperative Transaminases and Renal Function: A Meta-Analysis. World J Surg. 2016;40(12):2988-98. doi: 10.1007/s00268-016-3656-1
Wei X, Zheng W, Yang Z, Liu H, Tang T, Li X, et al. Effect of the intermittent Pringle maneuver on liver damage after hepatectomy: a retrospective cohort study. World J Surg Oncol [Internet]. 2019 [citado 18 Abr 2020];17(1):142. Disponible en: https://wjso.biomedcentral.com/articles/10.1186/s12957-019-1680-y
Petrone P, Magadan Alvarez C, Joseph D, Cartagena L, Ali F, Collin EMB. Approach and Management of Traumatic Retroperitoneal Injuries. Cir Esp. 2018;96(5):250-9. doi: 10.1016/j.ciresp.2018.02.021
Pikoulis E, Salem KM, Avgerinos ED, Pikouli A, Angelou A, Pikoulis A, et al. Damage Control for Vascular Trauma from the Prehospital to the Operating Room Setting. Front Surg [Internet]. 2017 [citado 18 Abr 2020];4:73. Disponible en: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5742177/. doi: 10.3389/fsurg.2017.00073
Feliciano DV. For the patient-Evolution in the management of vascular trauma. J Trauma Acute Care Surg. 2017;83(6):1205-12. doi: 10.1097/TA.0000000000001689
Yan H, Maximus S, Koopmann M, Keeley J, Smith B, Virgilio C, et al. Vascular Trauma Operative Experience is Inadequate in General Surgery Programs. Ann Vasc Surg. 2016;33:94-7. doi: 10.1016/j.avsg.2016.02.005
Etienne JH, Massalou D. Damage control surgery: Management of severe abdominal trauma (with video). J Visc Surg [Internet]. 2019 [citado 18 Abr 2020];156(1):64-6. Disponible en: https://www.sciencedirect.com/science/article/abs/pii/S187878861830119X?via%3Dihub doi: 10.1016/j.jviscsurg.2018.08.005
Akita M, Yamasaki N, Miyake T, Mimura K, Maeda E, Nishimura T, et al. Cattell-Braasch maneuver facilitates the artery-first approach and complete excision of the mesopancreas for pancreatoduodenectomy. J Surg Oncol [Internet]. 2020 [citado 18 Abr 2020];121(7):1126-31. Disponible en: https://onlinelibrary.wiley.com/doi/abs/10.1002/jso.25892
doi: 10.1002/jso.25892
Kobayashi LM, Costantini TW, Hamel MG, Dierksheide JE, Coimbra R. Abdominal vascular trauma. Trauma Surg Acute Care Open [Internet]. 2016 [citado 18 Abr 2020];1(1):e000015. Disponible en: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5891707/. doi: 10.1136/tsaco-2016-000015
Braña R, Chullmir R, Duarte J, Geragthy F, Cursi A, Cervini OE. Maniobra de Wiart-Vautrin-Kocher. Prensa médica argentina. 1983;70(18):809-12.
Teixeira PGR, Du Bose J. Surgical Management of Vascular Trauma. Surg Clin North Am. 2017;97(5):1133-55. doi: 10.1016/j.suc.2017.05.001
Petrone P, Rodríguez-Perdomo M, Pérez-Jiménez A, Ali F, Brathwaite CEM, Joseph DK. Pre-peritoneal pelvic packing for the management of life-threatening pelvic fractures. Eur J Trauma Emerg Surg. 2019 Jun;45(3):417-421. doi: 10.1007/s00068-018-1018-4
Brenner M, Inaba K, Aiolfi A, Du Bose J, Fabian T, Bee T, et al. Resuscitative Endovascular Balloon Occlusion of the Aorta and Resuscitative Thoracotomy in Select Patients with Hemorrhagic Shock: Early Results from the American Association for the Surgery of Trauma's Aortic Occlusion in Resuscitation for Trauma and Acute Care Surgery Registry. J Am Coll Surg. 2018;226(5):730-40. doi: 10.1016/j.jamcollsurg.2018.01.044
Wu D, Zhou X, Ye L, Gan J, Zhang M. Emergency department crowding and the performance of damage control resuscitation in major trauma patients with hemorrhagic shock. Acad Emerg Med. 2015;22(8):915-21. doi: 10.1111/acem.12726
Kheirabadi BS, Terrazas IB, Miranda N, Voelker AN, Klemcke HG, Brown AW, et al. Long-term consequences of abdominal aortic and junctional tourniquet for hemorrhage control. J Surg Res. 2018;231:99-108. doi: 10.1016/j.jss.2018.05.017
Martín-González I, Doménech-Dolz A, Ascaso-Arbona M, Rueda C, García-Valentín A. Abordajes quirúrgicos de aorta: visión práctica para residentes. Cirugía Cardiovascular. 2015;22(3):144-51. DOI: 10.1016/j.circv.2014.10.006
Szuba A, Jiménez Armenteros FM, Argote Camacho A, Capitán Vallvey JM. Técnicas quirúrgicas para el control de la hemorragia. Cir Andal [Internet]. 2019 [citado 18 Abr 2020];30(1):135-40. Disponible en: https://www.asacirujanos.com/admin/upfiles/revista/2019/Cir_Andal_vol30_n1_21.pdf
Du Bose J, Fabian T, Bee T, Moore LJ, Holcomb JB, Brenner M, et al. Contemporary Utilization of Resuscitative Thoracotomy: Results From the AAST Aortic Occlusion for Resuscitation in Trauma and Acute Care Surgery (AORTA) Multicenter Registry. Shock. 2018;50(4):414-20.
doi: 10.1097/SHK.0000000000001091
Du Bose JJ, Scalea TM, Brenner M, Skiada D, Inaba K, Cannon J, et al. The AAST prospective Aortic Occlusion for Resuscitation in Trauma and Acute Care Surgery (AORTA) registry: Data on contemporary utilization and outcomes of aortic occlusion and resuscitative balloon occlusion of the aorta (REBOA). J Trauma Acute Care Surg [Internet]. 2016 [citado 18 Abr 2020];81(3):409-19. Disponible en: https://journals.lww.com/jtrauma/Abstract/2016/09000/The_AAST_prospective_Aortic_Occlusion_for.1.aspx doi: 10.1097/TA.0000000000001079
Du Bose JJ, Savage SA, Fabian TC, Menaker J, Scalea T, Holcomb JB, et al. The American Association for the Surgery of Trauma Prospective Observational Vascular Injury Treatment (PROOVIT) registry: multicenter data on modern vascular injury diagnosis, management, and outcomes. J Trauma Acute Care Surg. 2015;78(2):215-22. doi: 10.1097/TA.0000000000000520
Faulconer ER, Branco BC, Loja MN, Grayson K, Sampson J, Fabian TC, et al. Use of open and endovascular surgical techniques to manage vascular injuries in the trauma setting: A review of the American Association for the Surgery of Trauma Prospective Observational Vascular Injury Trial registry. J Trauma Acute Care Surg. 2018;84(3):411-7. doi: 10.1097/TA.0000000000001776
Karaolanis G, Moris D, McCoy CC, Tsilimigras DI, Georgopoulos S, Bakoyiannis C. Contemporary Strategies in the Management of Civilian Abdominal Vascular Trauma. Front Surg [Internet]. 2018 [citado 18 Abr 2020];5:7. Disponible en: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5826055/.
doi: 10.3389/fsurg.2018.00007
Singh N, King DR, Feliciano DV. Major Abdominal Vascular Trauma. En: Martin MJ, Beekley AC, Eckert MJ, editors. Front Line Surgery: A Practical Approach. Cham: Springer International Publishing; 2017. p. 185-201.
Ju T, Rivas L, Kurland K, Chen S, Sparks A, Lin PP, et al. National trends in total vs subtotal gastrectomy for middle and distal third gastric cancer. Am J Surg. 2020;219(4):691-5. doi: 10.1016/j.amjsurg.2019.04.012
Zhang WH, Yang K, Chen XZ, Liu K, Chen XL, Zhao LY, et al. Effect of standardized surgical treatment and multidisciplinary treatment strategy on the prognosis of gastric cancer patients: report of a single-center cohort study. Zhonghua Wei Chang Wai Ke Za Zhi. 2020;23(4):396-404. doi: 10.3760/cma.j.cn.441530-20200224-00086
Enlaces refback
- No hay ningún enlace refback.

Esta obra está bajo una licencia de Creative Commons Reconocimiento-NoComercial 4.0 Internacional.















 06 julio 2025
06 julio 2025 La Revista está: Certificada por el CITMA
La Revista está: Certificada por el CITMA Acreditados como: "Web de Interés Sanitario"
Acreditados como: "Web de Interés Sanitario"
