Maniobras de movilización visceral en el trauma vascular abdominal
Resumen
Fundamento: el trauma vascular abdominal constituye un reto para el cirujano. El control vascular es una condición sine qua non en los pacientes que reciben intervención quirúrgica frente a esta letal enfermedad, donde las maniobras de movilización visceral constituyen una herramienta clave en el tratamiento.
Objetivo: explicar las maniobras de movilización visceral que pueden auxiliar al cirujano frente a un trauma vascular abdominal.
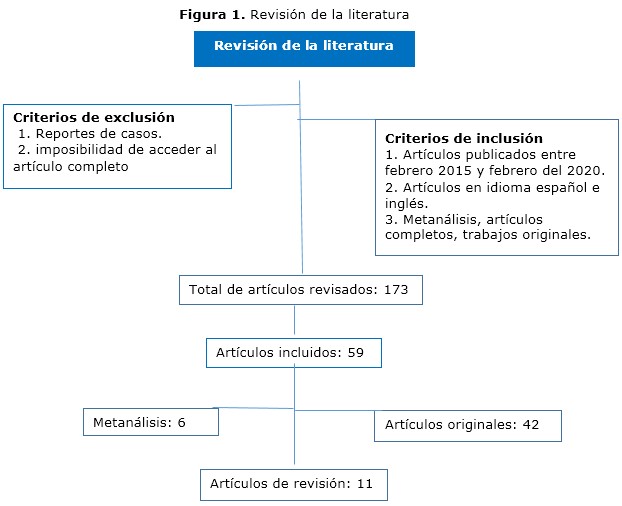
Métodos: se realizó una búsqueda en las bases de datos Scopus, Medline, Cochrane, Hinari y Redalyc se utilizaron los descriptores: trauma vascular, abdomen, maniobras, movilización visceral.
Resultados: se abordaron las maniobras de movilización visceral a tener en cuenta en el trauma vascular abdominal con una explicación de los principales pasos técnicos en cada una de ellas.
Conclusiones: el conocimiento y aplicación de las maniobras de movilización visceral constituyen una herramienta útil en el tratamiento de pacientes con trauma vascular abdominal.
DeCS: LESIONES DEL SISTEMA VASCULAR /cirugía; TRAUMATISMOS ABDOMINALES/complicaciones; VÍSCERAS/cirugía; PROCEDIMIENTOS QUIRÚRGICOS VASCULARES; PROCEDIMIENTOS QUIRÚRGICOS OPERATIVOS/métodos.
Descargas
Citas
1. Talbot E, Evans S, Hellenthal N, Monie D, Campbell P, Cooper S. Abdominal and Pelvic Vascular Injury: A National Trauma Data Bank Study. Am Surg [Internet]. 2019 [citado 18 Abr 2020];85(3):292-3. Disponible en: https://journals.sagepub.com/doi/10.1177/000313481908500335
doi.org/10.1177/000313481908500335
2. Warren KJ, Balogh ZJ. Major vascular trauma. Eur J Trauma Emerg Surg. 2019;45(6):941-2. doi: 10.1007/s00068-019-01267-2
3. Smith S, McAlister V, Parry N, Power A, Vogt K. Vascular trauma: Does experience in the United States apply to a Canadian centre? Can J Surg [Internet]. 2019 [citado 18 Abr 2020];62(6):499-501. Disponible en: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6877390/. doi: 10.1503/cjs.002317
4. D'Souza K, Bleszynski MS, Hawes HG. Rare constellation of abdominal vascular injuries in blunt trauma: Left gastric artery pseudoaneurysms and dissection. Int J Surg Case Rep [Internet]. 2019 [citado 18 Abr 2020];60:30-3. Disponible en: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6563334/.
doi: 10.1016/j.ijscr.2019.05.028
5. Avgerinos ED, Pikoulis E. Contemporary Strategies in the Management of Civilian Vascular Trauma. Front Surg [Internet]. 2018 [citado 18 Abr 2020];5:43. Disponible en: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6004396/.
doi: 10.3389/fsurg.2018.00043
6. Weale R, Kong V, Manchev V, Bekker W, Oosthuizen G, Brysiewicz P, et al. Management of intra-abdominal vascular injury in trauma laparotomy: a South African experience. Can J Surg [Internet]. 2018 [citado 18 Abr 2020];61(3):158-64. Disponible en: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5973903/.
doi: 10.1503/cjs.009717
7. Granite G, Pugh K, Chen H, Longinaker N, Garofalo E, Shackelford S, et al. Assessment of Anatomical Knowledge and Core Trauma Competency Vascular Skills. Mil Med [Internet]. 2018 [citado 18 Abr 2020];183(suppl 1):66-72. Disponible en: https://academic.oup.com/milmed/article-lookup/doi/10.1093/milmed/usx151 doi: 10.1093/milmed/usx151
8. Feliciano DV, Moore EE, Biffl WL. Western Trauma Association Critical Decisions in Trauma: Management of abdominal vascular trauma. J Trauma Acute Care Surg. 2015;79(6):1079-88. doi: 10.1097/TA.0000000000000869
9. Feliciano DV. Vascular Trauma Revisited. J Am Coll Surg [Internet]. 2018 [citado 18 Abr 2020];226(1):1-13. Disponible en: https://www.sciencedirect.com/science/article/abs/pii/S1072751517318422?via%3Dihub doi: 10.1016/j.jamcollsurg.2017.08.011
10. Pratschke S, Rauch A, Albertsmeier M, Rentsch M, Kirschneck M, Andrassy J, et al. Temporary Intraoperative Porto-Caval Shunts in Piggy-Back Liver Transplantation Reduce Intraoperative Blood Loss and Improve Postoperative Transaminases and Renal Function: A Meta-Analysis. World J Surg. 2016;40(12):2988-98. doi: 10.1007/s00268-016-3656-1
11. Wei X, Zheng W, Yang Z, Liu H, Tang T, Li X, et al. Effect of the intermittent Pringle maneuver on liver damage after hepatectomy: a retrospective cohort study. World J Surg Oncol [Internet]. 2019 [citado 18 Abr 2020];17(1):142. Disponible en: https://wjso.biomedcentral.com/articles/10.1186/s12957-019-1680-y
12. Petrone P, Magadan Alvarez C, Joseph D, Cartagena L, Ali F, Collin EMB. Approach and Management of Traumatic Retroperitoneal Injuries. Cir Esp. 2018;96(5):250-9. doi: 10.1016/j.ciresp.2018.02.021
13. Pikoulis E, Salem KM, Avgerinos ED, Pikouli A, Angelou A, Pikoulis A, et al. Damage Control for Vascular Trauma from the Prehospital to the Operating Room Setting. Front Surg [Internet]. 2017 [citado 18 Abr 2020];4:73. Disponible en: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5742177/. doi: 10.3389/fsurg.2017.00073
14. Feliciano DV. For the patient-Evolution in the management of vascular trauma. J Trauma Acute Care Surg. 2017;83(6):1205-12. doi: 10.1097/TA.0000000000001689
15. Yan H, Maximus S, Koopmann M, Keeley J, Smith B, Virgilio C, et al. Vascular Trauma Operative Experience is Inadequate in General Surgery Programs. Ann Vasc Surg. 2016;33:94-7. doi: 10.1016/j.avsg.2016.02.005
16. Etienne JH, Massalou D. Damage control surgery: Management of severe abdominal trauma (with video). J Visc Surg [Internet]. 2019 [citado 18 Abr 2020];156(1):64-6. Disponible en: https://www.sciencedirect.com/science/article/abs/pii/S187878861830119X?via%3Dihub doi: 10.1016/j.jviscsurg.2018.08.005
17. Akita M, Yamasaki N, Miyake T, Mimura K, Maeda E, Nishimura T, et al. Cattell-Braasch maneuver facilitates the artery-first approach and complete excision of the mesopancreas for pancreatoduodenectomy. J Surg Oncol [Internet]. 2020 [citado 18 Abr 2020];121(7):1126-31. Disponible en: https://onlinelibrary.wiley.com/doi/abs/10.1002/jso.25892
doi: 10.1002/jso.25892
18. Kobayashi LM, Costantini TW, Hamel MG, Dierksheide JE, Coimbra R. Abdominal vascular trauma. Trauma Surg Acute Care Open [Internet]. 2016 [citado 18 Abr 2020];1(1):e000015. Disponible en: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5891707/. doi: 10.1136/tsaco-2016-000015
19. Braña R, Chullmir R, Duarte J, Geragthy F, Cursi A, Cervini OE. Maniobra de Wiart-Vautrin-Kocher. Prensa médica argentina. 1983;70(18):809-12.
20. Teixeira PGR, Du Bose J. Surgical Management of Vascular Trauma. Surg Clin North Am. 2017;97(5):1133-55. doi: 10.1016/j.suc.2017.05.001
21. Petrone P, Rodríguez-Perdomo M, Pérez-Jiménez A, Ali F, Brathwaite CEM, Joseph DK. Pre-peritoneal pelvic packing for the management of life-threatening pelvic fractures. Eur J Trauma Emerg Surg. 2019 Jun;45(3):417-421. doi: 10.1007/s00068-018-1018-4
22. Brenner M, Inaba K, Aiolfi A, Du Bose J, Fabian T, Bee T, et al. Resuscitative Endovascular Balloon Occlusion of the Aorta and Resuscitative Thoracotomy in Select Patients with Hemorrhagic Shock: Early Results from the American Association for the Surgery of Trauma's Aortic Occlusion in Resuscitation for Trauma and Acute Care Surgery Registry. J Am Coll Surg. 2018;226(5):730-40. doi: 10.1016/j.jamcollsurg.2018.01.044
23. Wu D, Zhou X, Ye L, Gan J, Zhang M. Emergency department crowding and the performance of damage control resuscitation in major trauma patients with hemorrhagic shock. Acad Emerg Med. 2015;22(8):915-21. doi: 10.1111/acem.12726
24. Kheirabadi BS, Terrazas IB, Miranda N, Voelker AN, Klemcke HG, Brown AW, et al. Long-term consequences of abdominal aortic and junctional tourniquet for hemorrhage control. J Surg Res. 2018;231:99-108. doi: 10.1016/j.jss.2018.05.017
25. Martín-González I, Doménech-Dolz A, Ascaso-Arbona M, Rueda C, García-Valentín A. Abordajes quirúrgicos de aorta: visión práctica para residentes. Cirugía Cardiovascular. 2015;22(3):144-51. DOI: 10.1016/j.circv.2014.10.006
26. Szuba A, Jiménez Armenteros FM, Argote Camacho A, Capitán Vallvey JM. Técnicas quirúrgicas para el control de la hemorragia. Cir Andal [Internet]. 2019 [citado 18 Abr 2020];30(1):135-40. Disponible en: https://www.asacirujanos.com/admin/upfiles/revista/2019/Cir_Andal_vol30_n1_21.pdf
27. Du Bose J, Fabian T, Bee T, Moore LJ, Holcomb JB, Brenner M, et al. Contemporary Utilization of Resuscitative Thoracotomy: Results From the AAST Aortic Occlusion for Resuscitation in Trauma and Acute Care Surgery (AORTA) Multicenter Registry. Shock. 2018;50(4):414-20.
doi: 10.1097/SHK.0000000000001091
28. Du Bose JJ, Scalea TM, Brenner M, Skiada D, Inaba K, Cannon J, et al. The AAST prospective Aortic Occlusion for Resuscitation in Trauma and Acute Care Surgery (AORTA) registry: Data on contemporary utilization and outcomes of aortic occlusion and resuscitative balloon occlusion of the aorta (REBOA). J Trauma Acute Care Surg [Internet]. 2016 [citado 18 Abr 2020];81(3):409-19. Disponible en: https://journals.lww.com/jtrauma/Abstract/2016/09000/The_AAST_prospective_Aortic_Occlusion_for.1.aspx doi: 10.1097/TA.0000000000001079
29. Du Bose JJ, Savage SA, Fabian TC, Menaker J, Scalea T, Holcomb JB, et al. The American Association for the Surgery of Trauma Prospective Observational Vascular Injury Treatment (PROOVIT) registry: multicenter data on modern vascular injury diagnosis, management, and outcomes. J Trauma Acute Care Surg. 2015;78(2):215-22. doi: 10.1097/TA.0000000000000520
30. Faulconer ER, Branco BC, Loja MN, Grayson K, Sampson J, Fabian TC, et al. Use of open and endovascular surgical techniques to manage vascular injuries in the trauma setting: A review of the American Association for the Surgery of Trauma Prospective Observational Vascular Injury Trial registry. J Trauma Acute Care Surg. 2018;84(3):411-7. doi: 10.1097/TA.0000000000001776
31. Karaolanis G, Moris D, McCoy CC, Tsilimigras DI, Georgopoulos S, Bakoyiannis C. Contemporary Strategies in the Management of Civilian Abdominal Vascular Trauma. Front Surg [Internet]. 2018 [citado 18 Abr 2020];5:7. Disponible en: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5826055/.
doi: 10.3389/fsurg.2018.00007
32. Singh N, King DR, Feliciano DV. Major Abdominal Vascular Trauma. En: Martin MJ, Beekley AC, Eckert MJ, editors. Front Line Surgery: A Practical Approach. Cham: Springer International Publishing; 2017. p. 185-201.
33. Ju T, Rivas L, Kurland K, Chen S, Sparks A, Lin PP, et al. National trends in total vs subtotal gastrectomy for middle and distal third gastric cancer. Am J Surg. 2020;219(4):691-5. doi: 10.1016/j.amjsurg.2019.04.012
34. Zhang WH, Yang K, Chen XZ, Liu K, Chen XL, Zhao LY, et al. Effect of standardized surgical treatment and multidisciplinary treatment strategy on the prognosis of gastric cancer patients: report of a single-center cohort study. Zhonghua Wei Chang Wai Ke Za Zhi. 2020;23(4):396-404. doi: 10.3760/cma.j.cn.441530-20200224-00086
Publicado
Cómo citar
Número
Sección
Licencia
La Revista Archivo Medico Camagüey, ofrece de forma inmediata después de ser indexada en el Proyecto SciELO; acceso abierto al texto completo de los artículos bajo el principio de hacer disponible y gratuita la investigación para favorecer el intercambio del conocimiento global y coadyuvar a una mayor extensión, publicación, evaluación y uso extensivo de los artículos que se exponen pudiendo ser utilizados, sin fines comerciales, siempre y cuando se haga referencia a la fuente primaria.
Carta De Declaración De Autoría u Derechos De Autor(a)
Conflictos de intereses: los autores deberán declarar de forma obligatoria la presencia o no de conflictos de intereses en relación con la investigación presentada. (Descargar Plantilla para declarar confictos de intereses)
La Revista Archivo Médico Camagüey se encuentra bajo una
Licencia Creative Commons Reconocimiento-NoComercial 4.0 International (CC BY NC 4.0).
Esta licencia permite a otros distribuir, mezclar, ajustar y construir a partir de su obra, incluso con fines comerciales, siempre que le sea reconocida la autoría de la creación original. Esta es la licencia más servicial de las ofrecidas. Recomendada para una máxima difusión y utilización de los materiales sujetos a la licencia. La licencia completa puede consultarse en: https://creativecommons.org/licenses/












