SARS-COV-2: more than a respiratory virus
Keywords:
Coronavirus, COVID-19, SARS-CoV-2, fisiopatología, Manifestaciones Neurológicas, Enfermedades Cardiovasculares,Abstract
Background: the SARS-CoV-2 virus is responsible for the second pandemic of the 21st century. Since its appearance in China at the end of 2019, it has been associated with pneumonia and considered to be just another respiratory virus. However, during its global spread, it shows its ability to damage other organs with clinical manifestations never before described for other respiratory viruses.
Objective: to describe the scientific evidence that supports the direct extra-pulmonary damage produced by the SARS-CoV-2 virus in late stages of infection, which supports its biphasic nature and different from other respiratory viruses.
Methods: a search of the articles was carried out in the MEDLINE databases accessed from PubMed, SciELO and LILACS. Articles published in prepress repositories such as medRxiv, BioRxiv were also taken into account. Using the Mendeley reference manager and search manager, duplicates and those that did not meet the objective of the study were eliminated, selecting 63 articles for the present review.
Results: the evidence suggests that SARS-CoV-2 has a tropism not only limited to the respiratory tract. The clinical progression of COVID-19 presents a biphasic course, with flu-like manifestations in the first phase and post-acute and persistent episodes in the late phase, caused by direct damage to the central nervous, cardiovascular, endocrine and renal systems.
Conclusions: SARS-CoV-2 infection should not be considered only as an acute infection limited to the respiratory tract.
DeCS: SARS VIRUS/pathogenicity; CORONAVIRUS INFECTIONS/transmission; RESPIRATORY TRACT INFECTIONS/prevention & control; VIRAL TROPISM/physiology; VIRUS REPLICATION.
Downloads
References
1. World Health Organization. Timeline: WHO’s COVID-19 response [Internet]. Ginebra:WHO; 2020 [citado 22 Feb 2021]. Disponible en: https://bit.ly/3j1aOKF
2. Zheng KI, Feng G, Liu WY, Targher G, Byrne CD, Zheng MH. Extrapulmonary complications of COVID‐19: A multisystem disease? J Med Virol [Internet]. 2021 [citado 22 Feb 2021];93(1):323-335. Disponible en: https://doi.org/10.1002/jmv.26294
3. Yen CY, Wu WT, Chang CY, Wong YC, Lai CC, Chan YJ, et al. Viral etiologies of acute respiratory tract infections among hospitalized children-A comparison between single and multiple viral infections. J Microbiol Immunol Infect [Internet]. 2019 [citado 22 Feb 2021];52(6):902–10. Disponible en: https://doi.org/10.1016/j.jmii.2019.08.013
4. Kutter JS, Spronken MI, Fraaij PL, Fouchier RA, Herfst S. Transmission routes of respiratory viruses among humans. Curr Opin Virol [Internet]. 2018 [citado 22 Feb 2021];28:142–51. Disponible en: https://dx.doi.org/10.1016%2Fj.coviro.2018.01.001
5. Sellers SA, Hagan RS, Hayden FG, Fischer WA. The hidden burden of influenza: A review of the extra-pulmonary complications of influenza infection. Influenza Other Respi Viruses [Internet]. 2017 [citado 22 Feb 2021];11(5):372–93. Disponible en: https://doi.org/10.1111/irv.12470
6. Lowry K, Woodman A, Cook J, Evans DJ. Recombination in Enteroviruses Is a Biphasic Replicative Process Involving the Generation of Greater-than Genome Length Imprecise Intermediates. PLoS Pathog [Internet]. 2014 [citado 22 Feb 2021];10(6):e1004191. Disponible en: https://dx.doi.org/10.1371%2Fjournal.ppat.1004191
7. Charlton CL, Babady E, Ginocchio CC, Hatchette TF, Jerris RC, Li Y, et al. Practical Guidance for Clinical Microbiology Laboratories: Viruses Causing Acute Respiratory Tract Infections. Clin Microbiol Rev [Internet]. 2018;32(1): Disponible en: https://dx.doi.org/10.1128%2FCMR.00042-18
8. Kwong JC, Schwartz KL, Campitelli MA, Chung H, Crowcroft NS, Karnauchow T, et al. Acute Myocardial Infarction after Laboratory-Confirmed Influenza Infection. N Engl J Med [Internet]. 2018 [citado 22 Feb 2021];378(4):345–53. Disponible en: https://doi.org/10.1056/nejmoa1702090
9. Mejuto Fernández R. Complicaciones neurológicas asociadas al virus de la gripe [Tesis]. Cantabria: Universidad de Cantabria; 2015 [citado 22 Feb 2021]. Disponible en: https://repositorio.unican.es/xmlui/handle/10902/6795
10. Ing AJ, Cocks C, Green JP. COVID-19: in the footsteps of Ernest Shackleton. Thorax [Internet]. 2020 [citado 22 Feb 2021];75(8):693–4. Disponible en: http://dx.doi.org/10.1136/thoraxjnl-2020-215091
11. Sánchez-Oro R, Torres Nuez J, Martínez-Sanz G. La radiología en el diagnóstico de la neumonía por SARS-CoV-2 (COVID-19). Med Clin (Barc) [Internet]. 2020 [citado 22 Feb 2021];155(1):36-40. Disponible en: https://dx.doi.org/10.1016%2Fj.medcli.2020.03.004
12. Ooi EE, Low JG. Asymptomatic SARS-CoV-2 infection. Lancet Infect Dis [Internet]. 2020 [citado 22 Feb 2021];20(9):996–8. Disponible en: https://doi.org/10.1016/S1473-3099(20)30460-6
13. Dhama K, Khan S, Tiwari R, Sircar S, Bhat S, Malik YS, et al. Coronavirus Disease 2019-COVID-19. Clin Microbiol Rev [Internet]. 2020 [citado 22 Feb 2021];33(4):[aprox. 14 p.]. Disponible en: https://cmr.asm.org/content/cmr/33/4/e00028-20.full.pdf https://doi.org/10.1128/CMR.00028-20
14. Hu B, Huang S, Yin L. The cytokine storm and COVID‐19. J Med Virol [Internet]. 2021 [citado 22 Feb 2021];93(1):250-6. Disponible en: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7361342/pdf/JMV-9999-na.pdf https://doi.org/10.1002/jmv.26232
15. Gupta A, Madhavan M V, Sehgal K, Nair N, Mahajan S, Sehrawat TS, et al. Extrapulmonary manifestations of COVID-19. Nat Med [Internet]. 2020 [citado 22 Feb 2021];26(7):1017–32. Disponible en: https://doi.org/10.1038/s41591-020-0968-3
16. Wang K, Chen W, Zhou YS, Lian JQ, Zhang Z, Du P, et al. SARS-CoV-2 invades host cells via a novel route: CD147-spike protein. bioRxiv [Internet]. 2020 [citado 22 Feb 2021];3(14):988345. Disponible en: https://www.biorxiv.org/content/10.1101/2020.03.14.988345v1.full.pdf
17. Radzikowska U, Ding M, Tan G, Zhakparov D, Peng Y, Wawrzyniak P, et al. Distribution of ACE2, CD147, CD26, and other SARS‐CoV‐2 associated molecules in tissues and immune cells in health and in asthma, COPD, obesity, hypertension, and COVID‐19 risk factors. Allergy [Internet]. 2020 [citado 22 Feb 2021];75(11):2829-2845. Disponible en: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7300910/pdf/ALL-9999-na.pdf
doi: 10.1111/all.14429
18. Cantuti Castelvetri L, Ojha R, Pedro LD, Djannatian M, Franz J, Kuivanen S, et al. Neuropilin-1 facilitates SARS-CoV-2 cell entry and infectivity. Science [Internet]. 2020 [citado 22 Feb 2021];370(6518):856-860. Disponible en: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7857391/pdf/370_856.pdf
doi: 10.1126/science.abd2985
19. Jamal N, Whittier S, Carter RC, Zachariah P. Biphasic Variation Over Time in Presenting Features of Patients With COVID-19. Pediatrics [Internet]. 2020 [citado 22 Feb 2021];146(5):[aprox. 5 p.]. Disponible en: https://pediatrics.aappublications.org/content/pediatrics/146/5/e2020014902.full.pdf https://doi.org/10.1542/peds.2020-014902
20. Williamson EJ, Walker AJ, Bhaskaran K, Bacon S, Bates C, Morton CE, et al. Factors associated with COVID-19-related death using Open SAFELY. Nature [Internet]. 2020 [citado 22 Feb 2021];584(7821):430–6. Disponible en: https://doi.org/10.1038/s41586-020-2521-4
21. Carfì A, Bernabei R, Landi F. Persistent Symptoms in Patients After Acute COVID-19. JAMA [Internet]. 2020 [citado 22 Feb 2021];324(6):603. Disponible en: https://doi.org/10.1001/jama.2020.12603
22. Greenhalgh T, Knight M, A’Court C, Buxton M, Husain L. Management of post-acute covid-19 in primary care. BMJ [Internet]. 2020 [citado 22 Feb 2021];370:m3026. Disponible en: https://doi.org/10.1136/bmj.m3026
23. Gallagher J. Coronavirus: qué es la COVID-19 crónica y por qué a algunos les cuesta tanto recuperarse. BBC News [Internet]. 2020 [citado 22 Feb 2021]. Disponible en: https://www.bbc.com/mundo/noticias-54434271
24. Memoli MJ, Han A, Walters KA, Czajkowski L, Reed S, Athota R, et al. Influenza A Reinfection in Sequential Human Challenge: Implications for Protective Immunity and Universal Vaccine Development. Clin Infect Dis [Internet]. 2020 [citado 22 Feb 2021];70(5):748–53. Disponible en: https://doi.org/10.1093/cid/ciz281
25. Heinonen S, Jartti T, Garcia C, Oliva S, Smitherman C, Anguiano E, et al. Rhinovirus Detection in Symptomatic and Asymptomatic Children: Value of Host Transcriptome Analysis. Am J Respir Crit Care Med [Internet]. 2016 [citado 22 Feb 2021];193(7):772-82. Disponible en: https://dx.doi.org/10.1164%2Frccm.201504-0749OC
26. Tillett RL, Sevinsky JR, Hartley PD, Kerwin H, Crawford N, Gorzalski A, et al. Genomic evidence for reinfection with SARS-CoV-2: a case study. Lancet Infect Dis [Internet]. 2021 [citado 22 Feb 2021];21(1):52-58. Disponible en: https://doi.org/10.1016/S1473-3099(20)30764-7
27. Zlateva KT, de Vries JJC, Coenjaerts FEJ, van Loon AM, Verheij T, Little P, et al. Prolonged shedding of rhinovirus and re-infection in adults with respiratory tract illness. Eur Respir J [Internet]. 2014 [citado 22 Feb 2021];44(1):169-77. Disponible en: https://doi.org/10.1183/09031936.00172113
28. Vaira LA, Salzano G, Deiana G, De Riu G. Anosmia and Ageusia: Common Findings in COVID‐19 Patients. Laryngoscope [Internet]. 2020 [citado 22 Feb 2021];130(7):1787–1787. Disponible en: https://dx.doi.org/10.1002%2Flary.28692
29. Lechien JR, Chiesa Estomba CM, De Siati DR, Horoi M, Le Bon SD, Rodriguez A, et al. Olfactory and gustatory dysfunctions as a clinical presentation of mild-to-moderate forms of the coronavirus disease (COVID-19): a multicenter European study. Eur Arch Oto Rhino Laryngology [Internet]. 2020 [citado 22 Feb 2021];277(8):2251–61. Disponible en: https://dx.doi.org/10.1007%2Fs00405-020-05965-1
30. Vaira LA, Hopkins C, Petrocelli M, Lechien JR, Soma D, Giovanditto F, et al. Do olfactory and gustatory psychophysical scores have prognostic value in COVID-19 patients? A prospective study of 106 patients. J Otolaryngol Head Neck Surg [Internet]. 2020 [citado 22 Feb 2021];49(1):56. Disponible en: https://dx.doi.org/10.1186%2Fs40463-020-00449-y
31. Moriguchi T, Harii N, Goto J, Harada D, Sugawara H, Takamino J, et al. A first case of meningitis/encephalitis associated with SARS-Coronavirus-2. Int J Infect Dis [Internet]. 2020 [citado 22 Feb 2021];94:55-8. Disponible en: https://dx.doi.org/10.1016%2Fj.ijid.2020.03.062
32. Sharifian Dorche M, Huot P, Osherov M, Wen D, Saveriano A, Giacomini PS, et al. Neurological complications of coronavirus infection; a comparative review and lessons learned during the COVID-19 pandemic. J Neurol Sci [Internet]. 2020 [citado 22 Feb 2021];417:[aprox. 15 p.]. Disponible en: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7413162/pdf/main.pdf https://dx.doi.org/10.1016%2Fj.jns.2020.117085
33. Ellul MA, Benjamin L, Singh B, Lant S, Michael BD, Easton A, et al. Neurological associations of COVID-19. Lancet Neurol [Internet]. 2020 [citado 22 Feb 2021];19(9):767–83. Disponible en: https://dx.doi.org/10.1016%2FS1474-4422(20)30221-0
34. Najjar S, Najjar A, Chong DJ, Pramanik BK, Kirsch C, Kuzniecky RI, et al. Central nervous system complications associated with SARS-CoV-2 infection: integrative concepts of pathophysiology and case reports. J Neuroinflammation [Internet]. 2020 [citado 22 Feb 2021];17(1):231. Disponible en: https://dx.doi.org/10.1186%2Fs12974-020-01896-0
35. Holmes JL, Brake S, Docherty M, Lilford R, Watson S. Emergency ambulance services for heart attack and stroke during UK’s COVID-19 lockdown. Lancet [Internet]. 2020 [citado 22 Feb 2021];395(10237):e93–4. Disponible en: https://doi.org/10.1016/S0140-6736(20)31031-X
36. Xu Z, Shi L, Wang Y, Zhang J, Huang L, Zhang C, et al. Pathological findings of COVID-19 associated with acute respiratory distress syndrome. Lancet Respir Med [Internet]. 2020 [citado 22 Feb 2021];8(4):420–2. Disponible en: https://doi.org/10.1016/S2213-2600(20)30076-X
37. Dolhnikoff M, Ferreira Ferranti J, de Almeida Monteiro RA, Duarte-Neto AN, Soares Gomes-Gouvêa M, ViuDegaspare N, et al. SARS-CoV-2 in cardiac tissue of a child with COVID-19-related multisystem inflammatory syndrome. Lancet Child Adolesc Heal [Internet]. 2020 [citado 22 Feb 2021];4(10):790–4. Disponible en: https://doi.org/10.1016/S2352-4642(20)30257-1
38. Pirzada A, Mokhtar AT, Moeller AD. COVID-19 and Myocarditis: What Do We Know So Far? CJC Open [Internet]. 2020 [citado 22 Feb 2021];2(4):278-85. Disponible en: https://doi.org/10.1016/j.cjco.2020.05.005
39. Buja LM, Wolf DA, Zhao B, Akkanti B, McDonald M, Lelenwa L, et al. The emerging spectrum of cardiopulmonary pathology of the coronavirus disease 2019 (COVID-19): Report of 3 autopsies from Houston, Texas, and review of autopsy findings from other United States cities. Cardiovasc Pathol [Internet]. 2020 [citado 22 Feb 2021];48:107233. Disponible en: https://doi.org/10.1016/j.carpath.2020.107233
40. Bernal Torres W, Herrera Escandón Á, Hurtado Rivera M, Plata Mosquera CA. COVID-19 fulminant myocarditis: a case report. Eur Hear J Case Reports [Internet]. 2020 [citado 22 Feb 2021];4(FI1):1-6. Disponible en: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7454494/pdf/ytaa212.pdf https://doi.org/10.1093/ehjcr/ytaa212
41. Iacobellis G, Penaherrera CA, Bermudez LE, Bernal Mizrachi E. Admission hyperglycemia and radiological findings of SARS-CoV2 in patients with and without diabetes. Diabetes Res Clin Pract [Internet]. 2020 [citado 22 Feb 2021];164:108185. Disponible en: https://dx.doi.org/10.1016%2Fj.diabres.2020.108185
42. Bode B, Garrett V, Messler J, McFarland R, Crowe J, Booth R, et al. Glycemic Characteristics and Clinical Outcomes of COVID-19 Patients Hospitalized in the United States. J Diabetes SciTechnol [Internet]. 2020 [citado 22 Feb 2021];14(4):813–21. Disponible en: https://doi.org/10.1177%2F1932296820924469
43. Marik PE, Bellomo R. Stress hyperglycemia: an essential survival response! Crit Care [Internet]. 2013 [citado 22 Feb 2021];17(2):305. Disponible en: https://doi.org/10.1186/cc12514
44. Wei L, Sun S, Xu C, Zhang J, Xu Y, Zhu H, et al. Pathology of the thyroid in severe acute respiratory syndrome. Hum Pathol [Internet]. 2007 [citado 22 Feb 2021];38(1):95–102. Disponible en: https://doi.org/10.1016/j.humpath.2006.06.011
45. Yao XH, TY L. Histopathological study of new coronavirus pneumonia (COVID-19) in three patients. Chinese J Pathol [Internet]. 2020 [citado 22 Feb 2021];49. Disponible en: https://bit.ly/348pOCc
46. Vishvkarma R, Rajender S. Could SARS‐CoV‐2 affect male fertility? Andrologia [Internet]. 2020 [citado 22 Feb 2021];52(9). Disponible en: https://doi.org/10.1111/and.13712
47. Zupin L, Pascolo L, Zito G, Ricci G, Crovella S. SARS-CoV-2 and the next generations: which impact on reproductive tissues? J Assist Reprod Genet [Internet]. 2020 [citado 22 Feb 2021];37(10):2399–403. Disponible en: https://doi.org/10.1007/s10815-020-01917-0
48. Bunders MJ, Altfeld M. Implications of Sex Differences in Immunity for SARS-CoV-2 Pathogenesis and Design of Therapeutic Interventions. Immunity [Internet]. 2020 [citado 22 Feb 2021];53(3):487-95. Disponible en: https://doi.org/10.1016/j.immuni.2020.08.003
49. Li M-Y, Li L, Zhang Y, Wang X-S. Expression of the SARS-CoV-2 cell receptor gene ACE2 in a wide variety of human tissues. Infect Dis Poverty [Internet]. 2020 [citado 22 Feb 2021];9(1):45. Disponible en: https://doi.org/10.1186/s40249-020-00662-x
50. Ding Y, He L, Zhang Q, Huang Z, Che X, Hou J, et al. Organ distribution of severe acute respiratory syndrome(SARS) associated coronavirus (SARS-CoV) in SARS patients: implications for pathogenesis and virus transmission pathways. J Pathol [Internet]. 2004 [citado 22 Feb 2021];203(2):622-30. Disponible en: https://doi.org/10.1002/path.1560
51. Zinserling VA, Semenova NY, Markov AG, Rybalchenko O V, Wang J, Rodionov RN, et al. Inflammatory Cell Infiltration of Adrenals in COVID-19. Horm Metab Res [Internet]. 2020 [citado 22 Feb 2021];52(09):639-41. Disponible en: https://doi.org/10.1055/a-1191-8094
52. Su H, Yang M, Wan C, Yi L-X, Tang F, Zhu H-Y, et al. Renal histopathological analysis of 26 postmortem findings of patients with COVID-19 in China. Kidney Int [Internet]. 2020 [citado 22 Feb 2021];98(1):219–27. Disponible en: https://doi.org/10.1016/j.kint.2020.04.003
53. Schurink B, Roos E, Radonic T, Barbe E, Bouman CSC, de Boer HH, et al. Viral presence and immunopathology in patients with lethal COVID-19: a prospective autopsy cohort study. Lancet Microbe [Internet]. 2020 [citado 22 Feb 2021];1(7):[aprox. 8 p.]. Disponible en: https://doi.org/10.1016/S2666-5247(20)30144-0
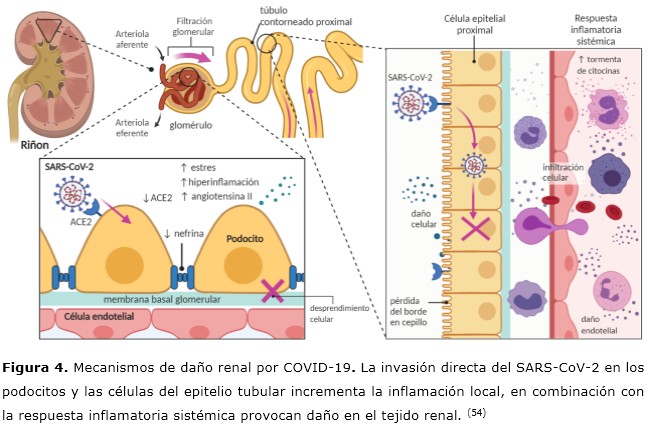
54. Martinez-Rojas MA, Vega-Vega O, Bobadilla NA. Is the kidney a target of SARS-CoV-2? Am J Physiol Physiol [Internet]. 2020 [citado 22 Feb 2021];318(6):F1454–62. Disponible en: https://doi.org/10.1152/ajprenal.00160.2020
55. Wang W, Xu Y, Gao R, Lu R, Han K, Wu G, et al. Detection of SARS-CoV-2 in Different Types of Clinical Specimens. JAMA [Internet]. 2020 [citado 22 Feb 2021];323(18):1843-1844. Disponible en: https://doi.org/10.1001/jama.2020.3786
56. Yu F, Yan L, Wang N, Yang S, Wang L, Tang Y, et al. Quantitative Detection and Viral Load Analysis of SARS-CoV-2 in Infected Patients. Clin Infect Dis [Internet]. 2020 [citado 22 Feb 2021];71(15):793–8. Disponible en: https://doi.org/10.1093/cid/ciaa345
57. Wölfel R, Corman VM, Guggemos W, Seilmaier M, Zange S, Müller MA, et al. Virological assessment of hospitalized patients with COVID-2019. Nature [Internet]. 2020 [citado 22 Feb 2021];581(7809):465–9. Disponible en: https://doi.org/10.1038/s41586-020-2196-x
58. Knoops K, Kikkert M, Worm SHE van den, Zevenhoven Dobbe JC, van der Meer Y, Koster AJ, et al. SARS-coronavirus replication is supported by a reticulovesicular network of modified endoplasmic reticulum. PLoSBiol [Internet]. 2008 [citado 22 Feb 2021];6(9):e226. Disponible en: https://doi.org/10.1371/journal.pbio.0060226
59. Baglivo M, Baronio M, Natalini G, Beccari T, Chiurazzi P, Fulcheri E, et al. Natural small molecules as inhibitors of coronavirus lipid-dependent attachment to host cells: a possible strategy for reducing SARS-COV-2 infectivity? Acta Biomed [Internet]. 2020 [citado 22 Feb 2021];91(1):161–4. Disponible en: https://dx.doi.org/10.23750%2Fabm.v91i1.9402
60. Tanida I, Fukasawa M, Ueno T, Kominami E, Wakita T, Hanada K. Knockdown of autophagy-related gene decreases the production of infectious Hepatitis C virus particles. Autophagy [Internet]. 2009 [citado 22 Feb 2021];5(7):937-45. Disponible en: https://doi.org/10.4161/auto.5.7.9243
61. Elrashdy F, Aljaddawi AA, Redwan EM, Uversky VN. On the potential role of exosomes in the COVID-19 reinfection/reactivation opportunity. J Biomol Struct Dyn [Internet]. 2020 [citado 22 Feb 2021];1-12. Disponible en: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7441802/pdf/TBSD_0_1790426.pdf https://dx.doi.org/10.1080%2F07391102.2020.1790426
62. Ou X, Liu Y, Lei X, Li P, Mi D, Ren L, et al. Characterization of spike glycoprotein of SARS-CoV-2 on virus entry and its immune cross-reactivity with SARS-CoV. Nat Commun [Internet]. 2020 [citado 22 Feb 2021];11(1):1620. Disponible en: https://doi.org/10.1038/s41467-020-15562-9
63. Xia S, Liu M, Wang C, Xu W, Lan Q, Feng S, et al. Inhibition of SARS-CoV-2 (previously 2019-nCoV) infection by a highly potent pan-coronavirus fusion inhibitor targeting its spike protein that harbors a high capacity to mediate membrane fusion. Cell Res [Internet]. 2020 [citado 22 Feb 2021];30(4):343–55. Disponible en: https://doi.org/10.1038/s41422-020-0305-x
Published
How to Cite
Issue
Section
License
Copyright (c) 2021 Franklin Rómulo Aguilar-Gamboa, Jorge Arturo Vega-Fernández, Danny Omar Suclupe-Campos

This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License.
Copyright: Camagüey Medical Archive Magazine, offers immediately after being indexed in the SciELO Project; Open access to the full text of the articles under the principle of making available and free the research to promote the exchange of global knowledge and contribute to a greater extension, publication, evaluation and extensive use of the articles that can be used without purpose As long as reference is made to the primary source.
Conflicts of interest: authors must declare in a mandatory manner the presence or not of conflicts of interest in relation to the investigation presented.
(Download Statement of potential conflicts of interest)
The Revista Archivo Médico de Camagüey is under a License Creative Commons Attribution-Noncommercial-No Derivative Works 4.0 International (CC BY 4.0).
This license allows others to distribute, to mix, to adjust and to build from its work, even for commercial purposes, as long as it is recognized the authorship of the original creation. This is the most helpful license offered. Recommended for maximum dissemination and use of licensed materials. The full license can be found at: https://creativecommons.org/licenses/












 22 julio 2025
22 julio 2025