Factores de riesgo asociados al agravamiento clínico de los pacientes ingresados con enfermedad de Alzhéimer
Resumen
Introducción: La principal causa de demencia degenerativa es la enfermedad de Alzhéimer. En la población cubana, una de cada cuatro personas de 65 años y más fallece por esta enfermedad u otra forma de demencia.
Objetivo: Identificar los factores de riesgo asociados al agravamiento clínico de los pacientes ingresados con enfermedad de Alzhéimer en el Hospital Psiquiátrico Universitario Rene Vallejo Ortiz entre enero de 2013 y diciembre de 2022.
Métodos: Se realizó un estudio observacional, descriptivo y transversal. El universo estuvo integrado por todos los pacientes ingresados en la mencionada institución asistencial y docente. La muestra no probabilística y a criterio de los autores la integraron 77 pacientes adultos con el diagnóstico de la enfermedad en el periodo de estudio señalado. Las historias clínicas fueron la fuente secundaria de información. Se utilizó estadística descriptiva e inferencial. La información se resumió en tablas y gráficos.
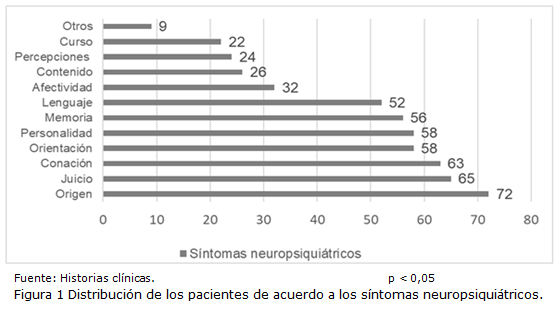
Resultados: El 90,6 % presentaban más de 60 años y más de la mitad eran del sexo masculino (54,5 %). La mayoría de los pacientes presentaron diversos síntomas asociados. Lo trastornos de personalidad y orientación se constataron en el 75,3 % mientras que los de memoria en el 72,7 %.
Conclusiones: El agravamiento clínico luego del ingreso hospitalario se acentuó en aquellos pacientes sin escolaridad, solteros, desocupados, con enfermedades cerebro vasculares y presencia de familias disfuncionales presentaron. Los pacientes anémicos o con signos de irritación cortical focal en región frontoparietal con generalización secundaria presentaron mayoritariamente un empeoramiento clínico.
DeCS: ENFERMEDAD DE ALZHÉIMER; PACIENTES INTERNOS; FACTORES DE RIESGO; DEMENCIA; SIGNOS Y SÍNTOMAS.
Descargas
Citas
1. Khan TK. An Algorithm for Preclinical Diagnosis of Alzheimer’s Disease. Front Neurosci [Internet]. 2018 [citado 15 Ago 2023];12:275. Disponible en: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5936981/pdf/fnins-12-00275.pdf
2. Pérez Rodríguez M, Álvarez Gómez T, Martínez Badaló EJ, Valdivia Cañizares S, Borroto Carpio I, Pedraza Núñez H. El síndrome del cuidador en cuidadores principales de ancianos con demencia Alzhéimer. Gac Méd Espirit [Internet] 2017 [citado 15 Ago 2023];19(1). Disponible en: https://revgmespirituana.sld.cu/index.php/gme/article/view/517/html
3. Tellechea P, Pujol N, Esteve-Belloch P, Echeveste B, García-Eulate MR, Arbizu J, et al. Early- and late-onset Alzheimer disease: Are they the same entity? Neurología [Internet]. 2018 [citado 15 Ago 2023];33(4):244-55. Disponible en: https://doaj.org/article/1d14674b8463488b82daef2893e4d4fa
4. Aranda M, Calabria A. Impacto económico-social de la enfermedad de Alzheimer. Neurol Arg [Internet]. 2019 Ene-Mar [citado 15 Ago 2023];11(1):19-26. Disponible en: https://www.elsevier.es/es-revista-neurologia-argentina-301-articulo-impacto-economico-social-enfermedad-alzheimer-S1853002818300831
5. Balea Fernández FJ, Alonso Ramírez J. Biomarcadores en la demencia tipo Alzheimer: sistema sanitario y edadismo. International Journal of Developmental and Educational Psychology [Internet]. 2020 [citado 15 Ago 2023];1(1):247-54. Disponible en: https://www.redalyc.org/journal/3498/349863388025/html/
6. Cubinkova V, Valachova B, Uhrinova I, Brezovakova V, Smolek T, Jadhav S, et al. Alternative hypotheses related to Alzheimer’s disease. Bratisl Lek Listy [Internet]. 2018 [citado 15 Ago 2023];119(4):210-16. Disponible en: http://www.elis.sk/download_file.php?product_id=5631&session_id=h7ntgagt03pvbn10a94l80h5k7
7. Romero-Vanegas SJ, Vargas-González JC, Pardo R, Eslava-Schmalbach J, Moreno- Angarita M. El sistema de salud colombiano y el reconocimiento de la enfermedad de Alzheimer. Rev Salud Pública [Internet]. 2021 [citado 15 Ago 2023];23(2):1-9. Disponible en: https://revistas.unal.edu.co/index.php/revsaludpublica/article/view/88369/82248
8. Nebel RA, Aggarwalb NT, Barnes LL, Gallaghera A, Goldsteinc JM, Kantarcie K, et al. Understanding the impact of sex and gender in Alzheimer's disease: A call to action. Alzheimers Dement [Internet]. 2018 Sep [citado 21 Ago 2023];14(9):1171-83. Disponible en: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6400070/
9. Espín Falcón JC. Factores de riesgo asociados a pacientes con enfermedad de Alzheimer y sus cuidadores principales. Rev cuban med gen integr [Internet]. 2020 [citado 15 Ago 2023];36(1). Disponible en: https://revmgi.sld.cu/index.php/mgi/article/view/1138
10.Prince M, Ali GC, Guerchet M, Prina AM, Albanese E, Wu YT. Recent global trends in the prevalence and incidence of dementia, and survival with dementia. Alzheimer’s Res Ther [Internet]. 2016 [citado 21 Ago 2023];8:23. Disponible en: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4967299/
11. Fiest KM, Roberts JI, Maxwell CJ, Hogan DB, Smith EE, Frolkis A, et al. The Prevalence and Incidence of Dementia Due to Alzheimer’s Disease: a Systematic Review and Meta-Analysis. Can J Neurol Sci [Internet] 2016 Abr [citado 21 Ago 2023];43(Suppl 1):S51-82. Disponible en: https://www.cambridge.org/core/journals/canadian-journal-of-neurological-sciences/article/prevalence-and-incidence-of-dementia-due-to-alzheimers-disease-a-systematic-review-and-metaanalysis/5456A8F9818DAE7764EFC942ADCF0A98
12. Seshadri S, Wolf PA, Beiser A, Au R, McNulty K, White R, et al. Lifetime risk of dementia and Alzheimer’s disease. The impact of mortality on risk estimates in the Framingham Study. Neurology [Internet]. 1997 Dic [citado 21 Ago 2023];49(6):1498-504. Disponible en: https://n.neurology.org/content/49/6/1498
13. Podcasy JL, Neill Epperson N. Considering sex and gender in Alzheimer disease and other dementias. Dialogues Clin Neurosci [Internet]. 2016 Dic [citado 21 Ago 2023];18(4):437-46. Disponible en: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5286729/
14. Pike CJ. Sex and the development of Alzheimer’s disease. J Neurosci Res [Internet]. 2017 Ene [citado 21 Ago 2023];95(1-2):671-80. Disponible en: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5120614/
15. Hakansson K, Rovio S, Helkala EL, Vilska AR, Winblad B, Soininen H, et al. Association between mid-life marital status and cognitive function in later life: population based cohort study. BMJ [Internet]. 2009 [citado 21 Ago 2023];339: b2462. Disponible en: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2714683/
16. Fan LY, Sun Y, Lee HJ, Yang SC, Chen TF, Lin KN, et al. Marital status, lifestyle and dementia: a Nationwide survey in Taiwan. PLoS One [Internet]. 2015 [citado 21 Ago 2023];10(9):e0139154. Disponible en: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4587383/
17. Sommerlad A, Ruegger J, Singh-Manoux A, Lewis G, Livingston G. Marriage and risk of dementia: systematic review and meta-analysis of observational studies. J Neurol Neurosurg Psychiatry [Internet]. 2018 Mar [citado 21 Ago 2023];89(3):231-8. Disponible en: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5869449/
18. Kobayashi E, Nakano M, Kubota K, Himuro N, Mizoguchi S, Chikenji T, et al. Activated forms of astrocytes with higher GLT-1 expression are associated with cognitive normal subjects with Alzheimer pathology in human brain. Sci Rep [Internet]. 2018 Ene [citado 21 Ago 2023];8(1):1712. Disponible en: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5786045/
19. Serrano-Pozoa A, Growdon JH. Is Alzheimer’s Disease Risk Modifiable? J Alzheimers Dis [Internet]. 2019 [citado 21 Ago 2023];67(3):795-819. Disponible en: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6708279/
20. Chhatwal JP, Schultz AP, Johnson KA, Hedden T, Jaimes S, Benzinger TLS, et al. Preferential degradation of cognitive networks differentiates Alzheimer’s disease from ageing. Brain [Internet]. 2018 May [citado 21 Ago 2023];141(5):1486-500. Disponible en: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5917745/
21. Lu FP, Lin KP, Kuo HK. Diabetes and the risk of multi-system aging phenotypes: a systematic review and meta-analysis. PLoS One [Internet]. 2009 [citado 15 Ago 2023]; 4(1): e4144. Disponible en: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2607544/
22. He W, Ruan Y, Yuan C, Luan X , He J. Hemoglobin, anemia, and poststroke cognitive impairment: A cohort study. Int J Geriatr Psychiatry [Internet]. 2020 May [citado 15 Ago 2023];35(5):564-71. Disponible en: https://onlinelibrary.wiley.com/doi/10.1002/gps.5272
23. Wolters FJ, Zonneveld HI, Licher S, Cremers LGM, Kamran Ikram M, Koudstaal PJ, et al. Hemoglobin and anemia in relation to dementia risk and accompanying changes on brain MRI. Neurology [Internet]. 2019 Ago [citado 15 Ago 2023];93(9):e917-e926. Disponible en: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6745727/
24. Bhat S, Acharya R, Dadmehr N, Adeli H. Clinical Neurophysiological and Automated EEG-Based Diagnosis of the Alzheimer’s Disease. Eur Neurol [Internet]. 2015 [citado 21 Ago 2023];74(3-4):202-10. Disponible en: https://karger.com/ene/article/74/3-4/202/125227/Clinical-Neurophysiological-and-Automated-EEG
Publicado
Cómo citar
Número
Sección
Licencia
Derechos de autor 2024 Wilson Antonio Pérez-Nicolaes, Ignacio Cabrera-Figueredo, Kelvis Dayron Castillo-Esquivel, María Georgina Nicolaes-Hernández, Grethel Camejo-Sampedro

Esta obra está bajo una licencia internacional Creative Commons Atribución-NoComercial 4.0.
La Revista Archivo Medico Camagüey, ofrece de forma inmediata después de ser indexada en el Proyecto SciELO; acceso abierto al texto completo de los artículos bajo el principio de hacer disponible y gratuita la investigación para favorecer el intercambio del conocimiento global y coadyuvar a una mayor extensión, publicación, evaluación y uso extensivo de los artículos que se exponen pudiendo ser utilizados, sin fines comerciales, siempre y cuando se haga referencia a la fuente primaria.
Carta De Declaración De Autoría u Derechos De Autor(a)
Conflictos de intereses: los autores deberán declarar de forma obligatoria la presencia o no de conflictos de intereses en relación con la investigación presentada. (Descargar Plantilla para declarar confictos de intereses)
La Revista Archivo Médico Camagüey se encuentra bajo una
Licencia Creative Commons Reconocimiento-NoComercial 4.0 International (CC BY NC 4.0).
Esta licencia permite a otros distribuir, mezclar, ajustar y construir a partir de su obra, incluso con fines comerciales, siempre que le sea reconocida la autoría de la creación original. Esta es la licencia más servicial de las ofrecidas. Recomendada para una máxima difusión y utilización de los materiales sujetos a la licencia. La licencia completa puede consultarse en: https://creativecommons.org/licenses/











