Fetal macrosomia and associated risk factors in Camagüey province
Abstract
Introduction: Fetal macrosomia has traditionally been defined by an arbitrary birth weight. Fetal macrosomia, whether defined by borderline weight or large for gestational age, is associated with numerous perinatal and maternal complications.
Objective: To describe the risk factors associated with fetal macrosomia in deliveries at Ana Betancourt de Mora Provincial Gyneco-Obstetric University Hospital during 2019.
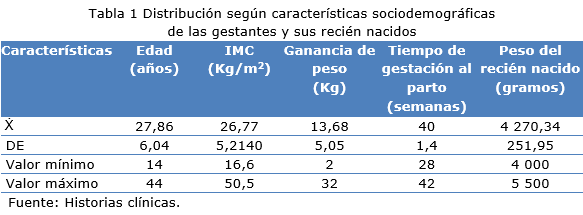
Methods: A cross-sectional descriptive observational study was carried out. The study universe was made up of all pregnant women who had newborns with a birth weight greater than or equal to 4 000 grams, which amounted to 526 pregnant women. Descriptive statistics were used. Average and standard deviation were calculated for the quantitative variables.
Results: The studied pregnant women had an average age of 27.86 years and an average BMI at uptake of 26.77 with an average value of weight gain of 13.68 Kg. Between 26 and 35 years there were 290 pregnant women with newborn macrosomic births, with respect to parity those who give birth without experience of this brought together 222 gravid women. In pregnant women classified as overweight with a gain of 10 to 15 kg, 104 of the macrosomic newborns are gathered. Regarding the type of delivery, cesarean section represented 61.4%. The presence of gestational or pregestational diabetes and preeclampsia, respectively, was observed in 40 pregnant women.
Conclusions: The excessive weight gain in pregnant women with nutritional evaluation of overweight or obese were those that had the highest incidence in the genesis of macrosomia in newborns.
DeCS: FETAL MACROSOMIA/diagnosis; OBESITY, MATERNAL; RISK FACTORS; NUTRITION ASSESSMENT; OBSTETRIC LABOR COMPLICATIONS.
Downloads
References
1. Jiménez Puñales S, Pentón Cortés RJ, Cairo González VM, Cabrera Blanco R, Chávez Betancourt LA, Álvarez Miranda MC. Factores de riesgo maternos y fetales en recién nacidos con macrosomía. Medicentro [Internet]. 2015 Jul-Sep [citado 30 Jun 2021];19(3):[aprox. 7 p.]. Disponible en: http://scielo.sld.cu/scielo.php?script=sci_arttext&pid=S1029-30432015000300002
2. American College of Obstetrics and Gynecologist. Fetal Macrosomia. Practice Bulletin [Internet]. 2016 [citado 30 Jun 2021];173:[aprox. 15 p.]. Disponible en: http://unmobgyn.pbworks.com/w/file/fetch/114688708/ACOGPracticeBulletin173FetalMacrosomia.pdf
3. Pacora Portella P. Macrosomía Fetal: Definición, Predicción, Riesgos y Prevención. Ginecol obstet [Internet]. 1993 [citado 30 Jun 2021];39(17):42-50. Disponible en: http://www.spog.org.pe/web/revista/index.php/RPGO/article/download/1633/pdf_173
4. Amini P, Maroufizadeh S, Hamidi O, Samani R, Sepidarkish M. Factors associated with macrosomia among singleton live-birth: A comparison between logistic regression, random forest and artificial neural network methods. Epidemiol Biostat Public Health [Internet]. Dic 2016 [citado 30 Jul 2021];13(4): [aprox. 8 p.]. Disponible en: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5936606/pdf/Int-J-Fertil-Steril-12-106.pdf
5. Yamamoto M, Insunza A. Macrosomía fetal. Contacto Científico [Internet]. 2016 [citado 30 Jul 2021];6(4):[aprox. 5 p.]. Disponible en: http://contactocientifico.alemana.cl/ojs/index.php/cc/ article/view/385
6. Romero Nardelli LB. Factores de riesgo asociados a la macrosomía fetal. Rev Nac (Itauguá) [Internet]. 2014 [citado 30 Jul 2021];6(1):16-24. Disponible en: http://scielo.iics.una.py/scielo.php?script=sci_abstract&pid=S2072-81742014000100003&lng=es&nrm=iso&tlng=es
7. Organización de las Naciones Unidas para la Alimentación y la Agricultura, Organización Panamericana de la Salud. Panorama de la seguridad alimentaria y nutricional en América Latina y el Caribe [Internet]. Santiago de Chile: FAO; 2016 [citado 30 Jun 2021]. 118 p. Disponible en: https://bit.ly/2iNev7I
8. Morais SS, Ide M, Moreno Morgan A, Garanhani Surita F. A novel body mass index reference range: an observational study. Clinics (Sao Paulo) [Internet]. 2017 Nov [citado 30 Jul 2021];72(11):698-707. Disponible en: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5706065/.
9. Toirac Lamarque AS, Pascual López V, Martínez Jiménez A, Area Suárez RI. Macrosomía fetal en madres no diabéticas. Caracterización mínima. MEDISAN [Internet]. 2013 Oct [citado 30 Jul 2021];17(10):[aprox. 11 p.]. Disponible en: http://scielo.sld.cu/scielo.php?script=sci_arttext&pid=S1029-30192013001000006
10. Rodríguez Fernández JM, Díaz Agüero H, Amador de Varona CI, Cabrera Figueredo I, Luaces Sánchez P, Cordoví Recio L. Caracterización materna-perinatal de las gestantes diabéticas. Arch méd Camagüey [Internet]. 2017 [citado 30 Jul 2021];21(1):[aprox. 10 p.]. Disponible en: http://scielo.sld.cu/pdf/amc/v21n1/amc100117.pdf
11. Alva Huaraj RA. Factores asociados a macrosomía en el recién nacido en el servicio de neonatología del hospital San José del Callao en el año 2017 [tesis]. Lima, Perú: Universidad Nacional Federico Villarreal; 2018 [citado 30 Jul 2021]. Disponible en: http://repositorio.unfv.edu.pe/handle/UNFV/1681
12. Koyanagi A, Zhang J, Dagvadorj A, Hirayama F, Shibuya K, Souza JP, et al. Macrosomia in 23 developing countries: analysis of a multicountry, facility- based, cross-sectional survey. Lancet [Internet]. 2013 Feb [citado 30 Jul 2021];381(9865):476-83. Disponible en: https://www.sciencedirect.com/science/article/abs/pii/S0140673612616055
13. Choukem SP, Njim T, Atashili J, Hamilton-Shield JP, Mbu R. High birth weight in a suburban hospital in Cameroon: an analysis of the clinical cut-off, prevalence, predictors and adverse outcomes. BMJ Open. 2016; 6(6). doi.org/10.1136/bmjopen-2016-011517
14. Baugh N, Harris DE, Aboueissa AM, Sarton C, Lichter E. The impact of maternal obesity and excessive gestational weight gain on maternal and infant outcomes in Maine: analysis of pregnancy risk assessment monitoring system results from 2000 to 2010. J Pregnancy [Internet]. 2016 [citado 30 Jul 2021];2016. Disponible en: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5055984/pdf/JP2016-5871313.pdf
15. Papazian T, Tayeh GA, Sibai D, Hout H, Melki I, Khabbaz LR. Impact of maternal body mass index and gestational weight gain on neonatal outcomes among healthy Middle-Eastern females. PloS One [Internet]. 2017 Jul [citado 30 Jul 2021]; 12(7): e0181255. Disponible en: https://pubmed.ncbi.nlm.nih.gov/28715482/.
16. Ledo Alves da Cunha AJ, Sobrino Toro M, Gutiérrez C, Alarcón Villaverde J. Prevalencia y factores asociados a macrosomía en Perú, 2013. Rev perú med exp salud publica [Internet]. 2017 Ene-Mar [citado 30 Jul 2021];34(1):[aprox. 6 p.]. Disponible en: http://www.scielo.org.pe/scielo.php?script=sci_arttext&pid=S1726-46342017000100006
17. Pacce S, Saure C, Mazza CS, Garcia S, Tomzig RG, Lopez AP, et al. Impact of maternal nutritional status before and during pregnancy on neonatal body composition: a cross-sectional study. Diabetes Metab Syndr [Internet]. 2016 Ene-Mar [citado 30 Jul 2021];10(1 Suppl 1):S7-S12. Disponible en: https://pubmed.ncbi.nlm.nih.gov/26431950/.
18. Lima RJCP, Batista RFL, Ribeiro MRC, Ribeiro CCC, Simões VME, Lima Neto PM, et al. Prepregnancy body mass index, gestational weight gain, and birth weight in the BRISA cohort. Rev Saude Publica [Internet]. 2018 [citado 30 Jul 2021];52:46. Disponible en: http://www.rsp.fsp.usp.br/wp-content/uploads/articles_xml/0034-8910-rsp-S1518-87872018052000125/0034-8910-rsp-S1518-87872018052000125.x83745.pdf
19. Diemert A, Lezius S, Pagenkemper M, Hansen G, Drozdowska A, Hetcher K, et al. Maternal nutrition, inadequate gestational weight gain and birth weight: results from a prospective birth cohort. BMC Pregnancy Childbirth [Internet]. 2016 Ago [citado 30 Jul 2021];16. Disponible en: https://bmcpregnancychildbirth.biomedcentral.com/track/pdf/10.1186/s12884-016-1012-y.pdf
20. García-De la Torre JI, Rodríguez-Valdez A, Delgado-Rosas A. Factores de riesgo de macrosomía fetal en pacientes sin diabetes mellitus gestacional. Ginecol Obstet Mex [Internet]. 2016 Mar [citado 30 Jul 2021];84(3):164-71. Disponible en: https://www.medigraphic.com/pdfs/ginobsmex/gom-2016/gom163f.pdf
Published
How to Cite
Issue
Section
License
Copyright (c) 2022 Ignacio Cabrera-Figueredo, José Manuel Rodríguez-Fernández, Jorge Luis Porrata-Mauri, Maurice José González-Basulto

This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License.
Copyright: Camagüey Medical Archive Magazine, offers immediately after being indexed in the SciELO Project; Open access to the full text of the articles under the principle of making available and free the research to promote the exchange of global knowledge and contribute to a greater extension, publication, evaluation and extensive use of the articles that can be used without purpose As long as reference is made to the primary source.
Conflicts of interest: authors must declare in a mandatory manner the presence or not of conflicts of interest in relation to the investigation presented.
(Download Statement of potential conflicts of interest)
The Revista Archivo Médico de Camagüey is under a License Creative Commons Attribution-Noncommercial-No Derivative Works 4.0 International (CC BY 4.0).
This license allows others to distribute, to mix, to adjust and to build from its work, even for commercial purposes, as long as it is recognized the authorship of the original creation. This is the most helpful license offered. Recommended for maximum dissemination and use of licensed materials. The full license can be found at: https://creativecommons.org/licenses/












 22 julio 2025
22 julio 2025