Utilidad y uso masivo de mascarillas frente a virus respiratorios: a propósito de la COVID-19
Palabras clave:
COVID-19, SARS-CoV-2, Equipo de Protección Personal, Mascarillas, Eficacia, Eficiencia, PoblaciónResumen
Fundamento: la COVID-19 se ha propagado con rapidez por todo el mundo y los estudios sobre el desarrollo de nuevos medicamentos y vacunas continúan en proceso. El uso de equipos de protección personal, el lavado de manos y el distanciamiento social, a la fecha son las principales medidas de defensa contra la infección.
Objetivo: describir la evidencia actual sobre la efectividad del uso de mascarillas de tela frente a las mascarillas quirúrgicas y respiradores, así como la eficacia del uso comunitario de mascarillas para controlar la propagación del SARS-CoV-2.
Métodos: se realizó una revisión de la literatura y análisis de la información utilizando los descriptores: COVID-19, SARS-CoV-2, personal protective equipment, masks, efficacy, efficiency, population. A partir de la información obtenida, se realizó una revisión bibliográfica de un total de 1 788 artículos publicados en las bases de datos MEDLINE/PubMed, SciELO y LILACS, sin restricciones de idioma se eliminaron los duplicados y aquellos que no se ajustaban al objetivo del estudio, seleccionando para la revisión 52 artículos.
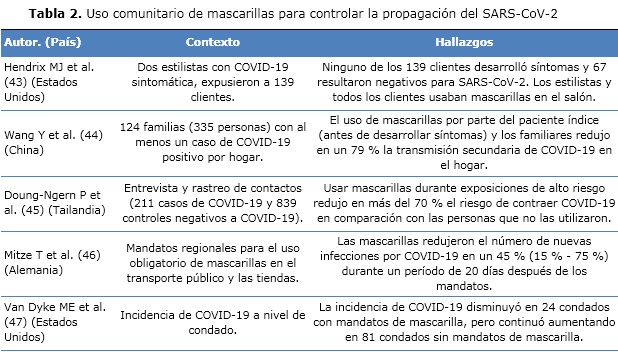
Resultados: existe mucha evidencia sobre el beneficio del uso continuo y masivo de mascarillas como herramienta para mitigar la transmisión de COVID-19 y otras enfermedades respiratorias en la comunidad. Las mascarillas de tela, de seguir las recomendaciones para su adecuada fabricación, ofrecen buena protección y su rendimiento es comparable al de las mascarillas quirúrgicas en la comunidad. Los respiradores deben ser reservados para el personal sanitario en el ámbito nosocomial, ya que ofrecen una apropiada protección en ambientes cerrados y de alta carga viral.
Conclusiones: el uso masivo de mascarillas puede complementar las estrategias de contención y prevención frente a enfermedades infecciosas de origen respiratorio incluida la COVID-19. Sin embargo, es necesario realizar más estudios específicos sobre el tema que ayuden a comprender mejor su rendimiento en campo.
DeCS: MÁSCARAS; EFICACIA; INFECCIONES POR CORONAVIRUS/prevención&control; ENFERMEDADES RESPIRATORIAS/prevención&control; POBLACIÓN.
Descargas
Citas
1. Verma S, Gustafsson A. Investigating the emerging COVID-19 research trends in the field of business and management: A bibliometric analysis approach. J Bus Res [Internet]. 2020 [citado 30 Ene 2021];118:253–61. Disponible en: https://doi.org/10.1016/j.jbusres.2020.06.057
2. Zaremba A, Aharon DY, Demir E, Kizys R, Zawadka D. COVID-19, government policy responses, and stock market liquidity around the world: A note. Res Int Bus Financ [Internet]. 2021 [citado 30 Ene 2021];56:101359. Disponible en: https://doi.org/10.1016/j.ribaf.2020.101359
3. Xiong J, Lipsitz O, Nasri F, Lui LMW, Gill H, Phan L, et al. Impact of COVID-19 pandemic on mental health in the general population: A systematic review. J Affect Disord [Internet]. 2020 [citado 30 Ene 2021];277:55-64. Disponible en: https://doi.org/10.1016/j.jad.2020.08.001
4. Sahebnasagh A, Avan R, Saghafi F, Mojtahedzadeh M, Sadremomtaz A, Arasteh O, et al. Pharmacological treatments of COVID-19. Pharmacol Reports [Internet]. 2020 [citado 30 Ene 2021];72(6):1446-78. Disponible en: https://doi.org/10.1007/s43440-020-00152-9
5. U.S.FOOD&DRUG. La FDA aprueba el primer tratamiento para el COVID-19 [Internet]. USA: FDA; c2020-21 [actualizado 22 Oct 2020; citado 30 Ene 2021]. Disponible en: https://www.fda.gov/news-events/press-announcements/la-fda-aprueba-el-primer-tratamiento-para-el-covid-19
6. Agility Logistics. Avigan® Approved for COVID-19 Treatment in Malaysia [Internet]. Dubai: Agility; ©2020 [actualizado 07 Dic 2020; citado 30 Ene 2021]. Disponible en: https://www.agility.com/en/avigan-approved-for-covid-19-treatment-in-malaysia/.
7. Matthay MA, Thompson BT. Dexamethasone in hospitalised patients with COVID-19: addressing uncertainties. Lancet Respir Med [Internet]. 2020 [citado 30 Ene 2021];8(12):1170-2. Disponible en: https://doi.org/10.1016/S2213-2600(20)30503-8
8. Xue X, Ball JK, Alexander C, Alexander MR. All Surfaces Are Not Equal in Contact Transmission of SARS-CoV-2. Matter [Internet]. 2020 [citado 30 Ene 2021];3(5):1433-41. Disponible en: https://doi.org/10.1016/j.matt.2020.10.006
9. Gierthmuehlen M, Kuhlenkoetter B, Parpaley Y, Gierthmuehlen S, Köhler D, Dellweg D. Evaluation and discussion of handmade face-masks and commercial diving-equipment as personal protection in pandemic scenarios. PLoS One [Internet]. 2020 [citado 30 Ene 2021];15(8):e0237899. Disponible en: https://dx.plos.org/10.1371/journal.pone.0237899
10. World Health Organization. Mask use in the context of COVID-19 [Internet]. USA: OMS; c2021 [actualizado 01 Dic 2020; citado 30 Ene 2021]. Disponible en: https://www.who.int/publications/i/item/advice-on-the-use-of-masks-in-the-community-during-home-care-and-in-healthcare-settings-in-the-context-of-the-novel-coronavirus-(2019-ncov)-outbreak
11. Kutter JS, Spronken MI, Fraaij PL, Fouchier RA, Herfst S. Transmission routes of respiratory viruses among humans. Curr Opin Virol [Internet]. 2018 [citado 30 Ene 2021];28:142-51. Disponible en: https://doi.org/10.1016/j.coviro.2018.01.001
12. Riddell S, Goldie S, Hill A, Eagles D, Drew TW. The effect of temperature on persistence of SARS-CoV-2 on common surfaces. Virol J [Internet]. 2020 [citado 30 Ene 2021];17(1):145. Disponible en: https://doi.org/10.1186/s12985-020-01418-7
13. The Lancet Respiratory Medicine. COVID-19 transmission—up in the air. Lancet Respir Med [Internet]. Dec 2020 [citado 30 Ene 2021];8(12):1159. Disponible en:
https://www.sciencedirect.com/journal/the-lancet-respiratory-medicine/vol/8/issue/12
14. Prather KA, Marr LC, Schooley RT, McDiarmid MA, Wilson ME, Milton DK. Airborne transmission of SARS-CoV-2. Science [Internet]. 2020 [citado 30 Ene 2021];370(6514):3032-304. Disponible en: https://www.science.org/doi/10.1126/science.abf0521?url_ver=Z39.88-2003&rfr_id=ori:rid:crossref.org&rfr_dat=cr_pub%20%200pubmed
15. Bartoszko JJ, Farooqi MAM, Alhazzani W, Loeb M. Medical masks vs N95 respirators for preventing COVID‐19 in healthcare workers: A systematic review and meta‐analysis of randomized trials. Influenza Other Respi Viruses [Internet]. 2020 [citado 30 Ene 2021];14(4):365-73. Disponible en: https://doi.org/10.1111/irv.12745
16. World Health Organization. Coronavirus disease (COVID-19): How is it transmitted? [Internet]. USA: OMS; c2021 [actualizado 13 Dic 2020; citado 30 Ene 2021]. Disponible en: https://www.who.int/emergencies/diseases/novel-coronavirus-2019/question-and-answers-hub/q-a-detail/coronavirus-disease-covid-19-how-is-it-transmitted
17. Centers for Disease Control and Prevention. How to Protect Yourself & Others [Internet]. USA: Department of Health & Human Services; 2020 [actualizado 13 Ago 2020; citado 30 Ene 2021]. Disponible en: https://www.cdc.gov/coronavirus/2019-ncov/prevent-getting-sick/prevention.html
18. Zhao T, Cheng C, Liu H, Sun C. Is one- or two-meters social distancing enough for COVID-19? Evidence for reassessing. Public Health [Internet]. 2020 [citado 30 Ene 2021];185:87. Disponible en: https://dx.doi.org/10.1016%2Fj.puhe.2020.06.005
19. Randerson J. UK to cut 2-meter social distance rule, says health secretary [Internet]. 2020 [citado 21 Jun 2021]. Disponible en: https://www.politico.eu/article/uk-to-cut-2-meter-social-distance-rule-says-health-secretary/.
20. Wise J. Covid-19: New coronavirus variant is identified in UK. BMJ [Internet]. 2020 [citado 30 Ene 2021];371:m4857. Disponible en: https://doi.org/10.1136/bmj.m4857
21. Conti P, Caraffa A, Gallenga CE, Kritas SK, Frydas I, Younes A, et al. The British variant of the new coronavirus-19 (Sars-Cov-2) should not create a vaccine problem. Journal of biological regulators and homeostatic agents [Internet]. 2021 [citado 30 Ene 2021];35. Disponible en: https://doi.org/10.23812/21-3-e
22. Eikenberry SE, Mancuso M, Iboi E, Phan T, Eikenberry K, Kuang Y, et al. To mask or not to mask: Modeling the potential for face mask use by the general public to curtail the COVID-19 pandemic. Infect Dis Model [Internet]. 2020 [citado 30 Ene 2021];5:293-308. Disponible en: https://doi.org/10.1016/j.idm.2020.04.001
23. O’Dowd K, Nair KM, Forouzandeh P, Mathew S, Grant J, Moran R, et al. Face Masks and Respirators in the Fight Against the COVID-19 Pandemic: A Review of Current Materials, Advances and Future Perspectives. Materials (Basel) [Internet]. 2020 [citado 30 Ene 2021];13(15):3363. Disponible en: https://dx.doi.org/10.3390%2Fma13153363
24. Centro para el desarrollo y prevención de las enfermedades. Guía interina para conservar y extender los suministros de mascarillas de respiración con filtro en sectores que no son de atención médica [Internet]. USA: Department of Health & Human Services; 2020 [actualizado 12 Abr 2020; citado 30 Ene 2021]. Disponible en: https://espanol.cdc.gov/coronavirus/2019-ncov/community/conserving-respirator-supply.html
25. Enright C. Las normas hacen posible... La protección de los trabajadores [Internet]. USA: ASTM International;©1996-2021 [citado 30 Ene 2021]. Disponible en: https://www.astm.org/SNEWS/SPANISH/SPMA12/enright_spma12.html
26. Centers for Disease Control and Prevention. How to Make Masks [Internet]. USA: Department of Health & Human Services; 2020 [actualizado 25 Oct 2020; citado 30 Ene 2021]. Disponible en: https://www.cdc.gov/coronavirus/2019-ncov/prevent-getting-sick/how-to-make-cloth-face-covering.html
27. Drewnick F, Pikmann J, Fachinger F, Moormann L, Sprang F, Borrmann S. Aerosol filtration efficiency of household materials for homemade face masks: Influence of material properties, particle size, particle electrical charge, face velocity, and leaks. Aerosol Sci Technol [Internet]. 2021 [citado 30 Ene 2021];55(1):63-79. Disponible en: https://doi.org/10.1080/02786826.2020.1817846
28. Li Y, Leung P, Yao L, Song QW, Newton E. Antimicrobial effect of surgical masks coated with nanoparticles. J Hosp Infect [Internet]. 2006 [citado 30 Ene 2021];62(1):58-63. Disponible en: https://doi.org/10.1016/j.jhin.2005.04.015
29. Akduman C, Akçakoca Kumbasar EP. Nanofibers in face masks and respirators to provide better protection. IOP Conf Ser Mater Sci Eng [Internet]. 2018 [citado 30 Ene 2021];460:12013. Disponible en: http://dx.doi.org/10.1088/1757-899X/460/1/012013
30. Ngonghala CN, Iboi E, Eikenberry S, Scotch M, MacIntyre CR, Bonds MH, et al. Mathematical assessment of the impact of non-pharmaceutical interventions on curtailing the 2019 novel Coronavirus. Math Biosci [Internet]. 2020 [citado 30 Ene 2021];325:108364. Disponible en: https://doi.org/10.1016/j.mbs.2020.108364
31. Chu DK, Akl EA, Duda S, Solo K, Yaacoub S, Schünemann HJ, et al. Physical distancing, face masks, and eye protection to prevent person-to-person transmission of SARS-CoV-2 and COVID-19: a systematic review and meta-analysis. Lancet [Internet]. 2020 [citado 30 Ene 2021];395(10242):1973-87. Disponible en: https://doi.org/10.1016/S0140-6736(20)31142-9
32. Radonovich LJ, Simberkoff MS, Bessesen MT, Brown AC, Cummings DAT, Gaydos CA, et al. N95 Respirators vs Medical Masks for Preventing Influenza Among Health Care Personnel: A Randomized Clinical Trial. JAMA [Internet]. 2019 [citado 30 Ene 2021];322(9):824-33. Disponible en: https://doi.org/10.1001/jama.2019.11645
33. Loeb M, Dafoe N, Mahony J, John M, Sarabia A, Glavin V, et al. Surgical Mask vs N95 Respirator for Preventing Influenza Among Health Care Workers. JAMA [Internet]. 2009 [citado 30 Ene 2021];302(17):1865. Disponible en: https://doi.org/10.1001/jama.2009.1466
34. Leung NHL, Chu DKW, Shiu EYC, Chan K-H, McDevitt JJ, Hau BJP, et al. Respiratory virus shedding in exhaled breath and efficacy of face masks. Nat Med [Internet]. 2020 [citado 30 Ene 2021];26(5):676-80. Disponible en: https://doi.org/10.1038/s41591-020-0843-2
35. Macintyre CR, Wang Q, Cauchemez S, Seale H, Dwyer DE, Yang P, et al. A cluster randomized clinical trial comparing fit-tested and non-fit-tested N95 respirators to medical masks to prevent respiratory virus infection in health care workers. Influenza Other Respi Viruses [Internet]. 2011 [citado 30 Ene 2021];5(3):170-9. Disponible en: https://dx.doi.org/10.1111%2Fj.1750-2659.2011.00198.x
36. Macintyre CR, Wang Q, Seale H, Yang P, Shi W, Gao Z, et al. A Randomized Clinical Trial of Three Options for N95 Respirators and Medical Masks in Health Workers. Am J Respir Crit Care Med [Internet]. 2013 [citado 30 Ene 2021];187(9):960-6. Disponible en: https://doi.org/10.1164/rccm.201207-1164oc
37. Ma Q, Shan H, Zhang H, Li G, Yang R, Chen J. Potential utilities of mask‐wearing and instant hand hygiene for fighting SARS‐CoV‐2. J Med Virol [Internet]. 2020 [citado 30 Ene 2021];92(9):1567-71. Disponible en: https://dx.doi.org/10.1002%2Fjmv.25805
38. Konda A, Prakash A, Moss GA, Schmoldt M, Grant GD, Guha S. Aerosol Filtration Efficiency of Common Fabrics Used in Respiratory Cloth Masks. ACS Nano [Internet]. 2020 [citado 30 Ene 2021];14(5):6339-47. Disponible en: https://doi.org/10.1021/acsnano.0c03252
39. Macintyre CR, Seale H, Dung TC, Hien NT, Nga PT, Chughtai AA, et al. A cluster randomised trial of cloth masks compared with medical masks in healthcare workers. BMJ Open [Internet]. 2015 [citado 30 Ene 2021];5(4):e006577-e006577. Disponible en: https://doi.org/10.1136/bmjopen-2014-006577
40. Davies A, Thompson K-A, Giri K, Kafatos G, Walker J, Bennett A. Testing the Efficacy of Homemade Masks: Would They Protect in an Influenza Pandemic? Disaster Med Public Health Prep [Internet]. 2013 [citado 30 Ene 2021];7(4):413-8. Disponible en: https://dx.doi.org/10.1017%2Fdmp.2013.43
41. Neupane BB, Mainali S, Sharma A, Giri B. Optical microscopic study of surface morphology and filtering efficiency of face masks. Peer J [Internet]. 2019 [citado 30 Ene 2021];7:e7142. Disponible en: https://dx.doi.org/10.7717%2Fpeerj.7142
42. Shakya KM, Noyes A, Kallin R, Peltier RE. Evaluating the efficacy of cloth facemasks in reducing particulate matter exposure. J Expo Sci Environ Epidemiol [Internet]. 2017 [citado 30 Ene 2021];27(3):352-7. Disponible en: https://doi.org/10.1038/jes.2016.42
43. Hendrix MJ, Walde C, Findley K, Trotman R. Absence of Apparent Transmission of SARS-CoV-2 from Two Stylists After Exposure at a Hair Salon with a Universal Face Covering Policy-Springfield, Missouri, May 2020. Morb Mortal Wkly Rep [Internet]. 2020 [citado 30 Ene 2021];69(28):930-2. Disponible en: https://doi.org/10.15585/mmwr.mm6928e2
44. Wang Y, Tian H, Zhang L, Zhang M, Guo D, Wu W, et al. Reduction of secondary transmission of SARS-CoV-2 in households by face mask use, disinfection and social distancing: a cohort study in Beijing, China. BMJ Glob Heal [Internet]. 2020 [citado 30 Ene 2021];5(5):e002794. Disponible en: https://doi.org/10.1136/bmjgh-2020-002794
45. Doung-Ngern P, Suphanchaimat R, Panjangampatthana A, Janekrongtham C, Ruampoom D, Daochaeng N, et al. Case-Control Study of Use of Personal Protective Measures and Risk for SARS-CoV 2 Infection, Thailand. Emerg Infect Dis [Internet]. 2020 [citado 30 Ene 2021];26(11):2607-16. Disponible en: https://doi.org/10.3201/eid2611.203003
46. Mitze T, Kosfeld R, Rode J, Wälde K. Face Masks Considerably Reduce COVID-19 Cases in Germany: A Synthetic Control Method Approach [Internet]. Germany: Institute of labor economics; Jun 2020 [citado 30 Ene 2021]. Disponible en: https://papers.ssrn.com/sol3/papers.cfm?abstract_id=3620634
47. Van Dyke ME, Rogers TM, Pevzner E, Satterwhite CL, Shah HB, Beckman WJ, et al. Trends in County-Level COVID-19 Incidence in Counties With and Without a Mask Mandate-Kansas, June 1–August 23, 2020. Morb Mortal Wkly Rep [Internet]. 2020 [citado 30 Ene 2021];69(47):1777-81. Disponible en: https://dx.doi.org/10.15585%2Fmmwr.mm6947e2
48. Wang J, Pan L, Tang S, Ji JS, Shi X. Mask use during COVID-19: A risk adjusted strategy. Environ Pollut [Internet]. 2020 [citado 30 Ene 2021];266:115099. Disponible en: https://dx.doi.org/10.1016%2Fj.envpol.2020.115099
49. BBC News Mundo. Mascarillas contra el coronavirus: cómo el rechazo al tapabocas une a la extrema derecha y la extrema izquierda [Internet]. USA: BBC News Mundo; ©2021 [citado 30 Ene 2021]. Disponible en: https://www.bbc.com/mundo/noticias-internacional-53810072
50. Kwon K-S, Park J-I, Park YJ, Jung D-M, Ryu K-W, Lee J-H. Evidence of Long-Distance Droplet Transmission of SARS-CoV-2 by Direct Air Flow in a Restaurant in Korea. J Korean Med Sci [Internet]. 2020 [citado 30 Ene 2021];35(46). Disponible en: https://jkms.org/DOIx.php?id=10.3346/jkms.2020.35.e415
51. Lu J, Gu J, Li K, Xu C, Su W, Lai Z, et al. COVID-19 Outbreak Associated with Air Conditioning in Restaurant, Guangzhou, China, 2020. Emerg Infect Dis [Internet]. 2020 [citado 30 Ene 2021];26(7):1628-31. Disponible en: https://doi.org/10.3201/eid2607.200764
52. Park SY, Kim Y-M, Yi S, Lee S, Na B-J, Kim CB, et al. Coronavirus Disease Outbreak in Call Center, South Korea. Emerg Infect Dis [Internet]. 2020 [citado 30 Ene 2021];26(8):1666-70. Disponible en: https://www.ncbi.nlm.nih.gov/pmc/articles/pmid/32324530/.
Publicado
Cómo citar
Número
Sección
Licencia
Derechos de autor 2021 Franklin Rómulo Aguilar-Gamboa, Danny Omar Suclupe-Campos

Esta obra está bajo una licencia internacional Creative Commons Atribución-NoComercial 4.0.
La Revista Archivo Medico Camagüey, ofrece de forma inmediata después de ser indexada en el Proyecto SciELO; acceso abierto al texto completo de los artículos bajo el principio de hacer disponible y gratuita la investigación para favorecer el intercambio del conocimiento global y coadyuvar a una mayor extensión, publicación, evaluación y uso extensivo de los artículos que se exponen pudiendo ser utilizados, sin fines comerciales, siempre y cuando se haga referencia a la fuente primaria.
Carta De Declaración De Autoría u Derechos De Autor(a)
Conflictos de intereses: los autores deberán declarar de forma obligatoria la presencia o no de conflictos de intereses en relación con la investigación presentada. (Descargar Plantilla para declarar confictos de intereses)
La Revista Archivo Médico Camagüey se encuentra bajo una
Licencia Creative Commons Reconocimiento-NoComercial 4.0 International (CC BY NC 4.0).
Esta licencia permite a otros distribuir, mezclar, ajustar y construir a partir de su obra, incluso con fines comerciales, siempre que le sea reconocida la autoría de la creación original. Esta es la licencia más servicial de las ofrecidas. Recomendada para una máxima difusión y utilización de los materiales sujetos a la licencia. La licencia completa puede consultarse en: https://creativecommons.org/licenses/











