Visceral mobilization maneuvers in abdominal vascular trauma
Abstract
Background: abdominal vascular trauma is a challenge for the surgeon. Vascular control is a sine qua non condition in patients who receive surgical intervention against this lethal pathology, where visceral mobilization maneuvers are a key tool in treatment.
Objective: to explain the visceral mobilization maneuvers that can help the surgeon against abdominal vascular trauma.
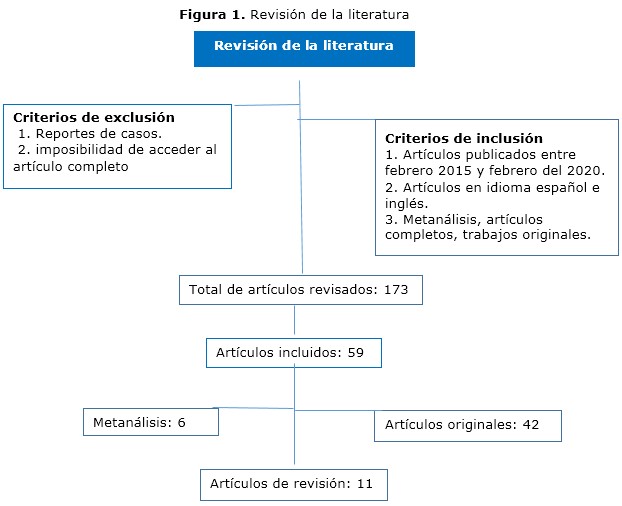
Methods: a search of the Scopus, Medline, Cochrane, Hinari and Redalyc databases was performed using the descriptors: vascular trauma, abdomen, maneuvers, visceral mobilization.
Results: visceral mobilization maneuvers to be taken into account in abdominal vascular trauma were addressed with an explanation of the main technical steps in each of them.
Conclusions: the knowledge and application of visceral mobilization maneuvers constitute a useful tool in the treatment of patients with abdominal vascular trauma.
DeCS: VASCULAR SYSTEM INJURIES/surgery; ABDOMINAL INJURIES/ complications; VISCERA /surgery; VASCULAR SURGICAL PROCEDURES; SURGICAL PROCEDURES, OPERATIVE /methods.
Downloads
References
1. Talbot E, Evans S, Hellenthal N, Monie D, Campbell P, Cooper S. Abdominal and Pelvic Vascular Injury: A National Trauma Data Bank Study. Am Surg [Internet]. 2019 [citado 18 Abr 2020];85(3):292-3. Disponible en: https://journals.sagepub.com/doi/10.1177/000313481908500335
doi.org/10.1177/000313481908500335
2. Warren KJ, Balogh ZJ. Major vascular trauma. Eur J Trauma Emerg Surg. 2019;45(6):941-2. doi: 10.1007/s00068-019-01267-2
3. Smith S, McAlister V, Parry N, Power A, Vogt K. Vascular trauma: Does experience in the United States apply to a Canadian centre? Can J Surg [Internet]. 2019 [citado 18 Abr 2020];62(6):499-501. Disponible en: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6877390/. doi: 10.1503/cjs.002317
4. D'Souza K, Bleszynski MS, Hawes HG. Rare constellation of abdominal vascular injuries in blunt trauma: Left gastric artery pseudoaneurysms and dissection. Int J Surg Case Rep [Internet]. 2019 [citado 18 Abr 2020];60:30-3. Disponible en: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6563334/.
doi: 10.1016/j.ijscr.2019.05.028
5. Avgerinos ED, Pikoulis E. Contemporary Strategies in the Management of Civilian Vascular Trauma. Front Surg [Internet]. 2018 [citado 18 Abr 2020];5:43. Disponible en: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6004396/.
doi: 10.3389/fsurg.2018.00043
6. Weale R, Kong V, Manchev V, Bekker W, Oosthuizen G, Brysiewicz P, et al. Management of intra-abdominal vascular injury in trauma laparotomy: a South African experience. Can J Surg [Internet]. 2018 [citado 18 Abr 2020];61(3):158-64. Disponible en: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5973903/.
doi: 10.1503/cjs.009717
7. Granite G, Pugh K, Chen H, Longinaker N, Garofalo E, Shackelford S, et al. Assessment of Anatomical Knowledge and Core Trauma Competency Vascular Skills. Mil Med [Internet]. 2018 [citado 18 Abr 2020];183(suppl 1):66-72. Disponible en: https://academic.oup.com/milmed/article-lookup/doi/10.1093/milmed/usx151 doi: 10.1093/milmed/usx151
8. Feliciano DV, Moore EE, Biffl WL. Western Trauma Association Critical Decisions in Trauma: Management of abdominal vascular trauma. J Trauma Acute Care Surg. 2015;79(6):1079-88. doi: 10.1097/TA.0000000000000869
9. Feliciano DV. Vascular Trauma Revisited. J Am Coll Surg [Internet]. 2018 [citado 18 Abr 2020];226(1):1-13. Disponible en: https://www.sciencedirect.com/science/article/abs/pii/S1072751517318422?via%3Dihub doi: 10.1016/j.jamcollsurg.2017.08.011
10. Pratschke S, Rauch A, Albertsmeier M, Rentsch M, Kirschneck M, Andrassy J, et al. Temporary Intraoperative Porto-Caval Shunts in Piggy-Back Liver Transplantation Reduce Intraoperative Blood Loss and Improve Postoperative Transaminases and Renal Function: A Meta-Analysis. World J Surg. 2016;40(12):2988-98. doi: 10.1007/s00268-016-3656-1
11. Wei X, Zheng W, Yang Z, Liu H, Tang T, Li X, et al. Effect of the intermittent Pringle maneuver on liver damage after hepatectomy: a retrospective cohort study. World J Surg Oncol [Internet]. 2019 [citado 18 Abr 2020];17(1):142. Disponible en: https://wjso.biomedcentral.com/articles/10.1186/s12957-019-1680-y
12. Petrone P, Magadan Alvarez C, Joseph D, Cartagena L, Ali F, Collin EMB. Approach and Management of Traumatic Retroperitoneal Injuries. Cir Esp. 2018;96(5):250-9. doi: 10.1016/j.ciresp.2018.02.021
13. Pikoulis E, Salem KM, Avgerinos ED, Pikouli A, Angelou A, Pikoulis A, et al. Damage Control for Vascular Trauma from the Prehospital to the Operating Room Setting. Front Surg [Internet]. 2017 [citado 18 Abr 2020];4:73. Disponible en: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5742177/. doi: 10.3389/fsurg.2017.00073
14. Feliciano DV. For the patient-Evolution in the management of vascular trauma. J Trauma Acute Care Surg. 2017;83(6):1205-12. doi: 10.1097/TA.0000000000001689
15. Yan H, Maximus S, Koopmann M, Keeley J, Smith B, Virgilio C, et al. Vascular Trauma Operative Experience is Inadequate in General Surgery Programs. Ann Vasc Surg. 2016;33:94-7. doi: 10.1016/j.avsg.2016.02.005
16. Etienne JH, Massalou D. Damage control surgery: Management of severe abdominal trauma (with video). J Visc Surg [Internet]. 2019 [citado 18 Abr 2020];156(1):64-6. Disponible en: https://www.sciencedirect.com/science/article/abs/pii/S187878861830119X?via%3Dihub doi: 10.1016/j.jviscsurg.2018.08.005
17. Akita M, Yamasaki N, Miyake T, Mimura K, Maeda E, Nishimura T, et al. Cattell-Braasch maneuver facilitates the artery-first approach and complete excision of the mesopancreas for pancreatoduodenectomy. J Surg Oncol [Internet]. 2020 [citado 18 Abr 2020];121(7):1126-31. Disponible en: https://onlinelibrary.wiley.com/doi/abs/10.1002/jso.25892
doi: 10.1002/jso.25892
18. Kobayashi LM, Costantini TW, Hamel MG, Dierksheide JE, Coimbra R. Abdominal vascular trauma. Trauma Surg Acute Care Open [Internet]. 2016 [citado 18 Abr 2020];1(1):e000015. Disponible en: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5891707/. doi: 10.1136/tsaco-2016-000015
19. Braña R, Chullmir R, Duarte J, Geragthy F, Cursi A, Cervini OE. Maniobra de Wiart-Vautrin-Kocher. Prensa médica argentina. 1983;70(18):809-12.
20. Teixeira PGR, Du Bose J. Surgical Management of Vascular Trauma. Surg Clin North Am. 2017;97(5):1133-55. doi: 10.1016/j.suc.2017.05.001
21. Petrone P, Rodríguez-Perdomo M, Pérez-Jiménez A, Ali F, Brathwaite CEM, Joseph DK. Pre-peritoneal pelvic packing for the management of life-threatening pelvic fractures. Eur J Trauma Emerg Surg. 2019 Jun;45(3):417-421. doi: 10.1007/s00068-018-1018-4
22. Brenner M, Inaba K, Aiolfi A, Du Bose J, Fabian T, Bee T, et al. Resuscitative Endovascular Balloon Occlusion of the Aorta and Resuscitative Thoracotomy in Select Patients with Hemorrhagic Shock: Early Results from the American Association for the Surgery of Trauma's Aortic Occlusion in Resuscitation for Trauma and Acute Care Surgery Registry. J Am Coll Surg. 2018;226(5):730-40. doi: 10.1016/j.jamcollsurg.2018.01.044
23. Wu D, Zhou X, Ye L, Gan J, Zhang M. Emergency department crowding and the performance of damage control resuscitation in major trauma patients with hemorrhagic shock. Acad Emerg Med. 2015;22(8):915-21. doi: 10.1111/acem.12726
24. Kheirabadi BS, Terrazas IB, Miranda N, Voelker AN, Klemcke HG, Brown AW, et al. Long-term consequences of abdominal aortic and junctional tourniquet for hemorrhage control. J Surg Res. 2018;231:99-108. doi: 10.1016/j.jss.2018.05.017
25. Martín-González I, Doménech-Dolz A, Ascaso-Arbona M, Rueda C, García-Valentín A. Abordajes quirúrgicos de aorta: visión práctica para residentes. Cirugía Cardiovascular. 2015;22(3):144-51. DOI: 10.1016/j.circv.2014.10.006
26. Szuba A, Jiménez Armenteros FM, Argote Camacho A, Capitán Vallvey JM. Técnicas quirúrgicas para el control de la hemorragia. Cir Andal [Internet]. 2019 [citado 18 Abr 2020];30(1):135-40. Disponible en: https://www.asacirujanos.com/admin/upfiles/revista/2019/Cir_Andal_vol30_n1_21.pdf
27. Du Bose J, Fabian T, Bee T, Moore LJ, Holcomb JB, Brenner M, et al. Contemporary Utilization of Resuscitative Thoracotomy: Results From the AAST Aortic Occlusion for Resuscitation in Trauma and Acute Care Surgery (AORTA) Multicenter Registry. Shock. 2018;50(4):414-20.
doi: 10.1097/SHK.0000000000001091
28. Du Bose JJ, Scalea TM, Brenner M, Skiada D, Inaba K, Cannon J, et al. The AAST prospective Aortic Occlusion for Resuscitation in Trauma and Acute Care Surgery (AORTA) registry: Data on contemporary utilization and outcomes of aortic occlusion and resuscitative balloon occlusion of the aorta (REBOA). J Trauma Acute Care Surg [Internet]. 2016 [citado 18 Abr 2020];81(3):409-19. Disponible en: https://journals.lww.com/jtrauma/Abstract/2016/09000/The_AAST_prospective_Aortic_Occlusion_for.1.aspx doi: 10.1097/TA.0000000000001079
29. Du Bose JJ, Savage SA, Fabian TC, Menaker J, Scalea T, Holcomb JB, et al. The American Association for the Surgery of Trauma Prospective Observational Vascular Injury Treatment (PROOVIT) registry: multicenter data on modern vascular injury diagnosis, management, and outcomes. J Trauma Acute Care Surg. 2015;78(2):215-22. doi: 10.1097/TA.0000000000000520
30. Faulconer ER, Branco BC, Loja MN, Grayson K, Sampson J, Fabian TC, et al. Use of open and endovascular surgical techniques to manage vascular injuries in the trauma setting: A review of the American Association for the Surgery of Trauma Prospective Observational Vascular Injury Trial registry. J Trauma Acute Care Surg. 2018;84(3):411-7. doi: 10.1097/TA.0000000000001776
31. Karaolanis G, Moris D, McCoy CC, Tsilimigras DI, Georgopoulos S, Bakoyiannis C. Contemporary Strategies in the Management of Civilian Abdominal Vascular Trauma. Front Surg [Internet]. 2018 [citado 18 Abr 2020];5:7. Disponible en: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5826055/.
doi: 10.3389/fsurg.2018.00007
32. Singh N, King DR, Feliciano DV. Major Abdominal Vascular Trauma. En: Martin MJ, Beekley AC, Eckert MJ, editors. Front Line Surgery: A Practical Approach. Cham: Springer International Publishing; 2017. p. 185-201.
33. Ju T, Rivas L, Kurland K, Chen S, Sparks A, Lin PP, et al. National trends in total vs subtotal gastrectomy for middle and distal third gastric cancer. Am J Surg. 2020;219(4):691-5. doi: 10.1016/j.amjsurg.2019.04.012
34. Zhang WH, Yang K, Chen XZ, Liu K, Chen XL, Zhao LY, et al. Effect of standardized surgical treatment and multidisciplinary treatment strategy on the prognosis of gastric cancer patients: report of a single-center cohort study. Zhonghua Wei Chang Wai Ke Za Zhi. 2020;23(4):396-404. doi: 10.3760/cma.j.cn.441530-20200224-00086
Published
How to Cite
Issue
Section
License
Copyright (c) 2021 Miguel Emilio García-Rodríguez, Miguel Javier García-Basulto, Raul Koelig-Padrón, Arian Benavidez-Márquez

This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License.
Copyright: Camagüey Medical Archive Magazine, offers immediately after being indexed in the SciELO Project; Open access to the full text of the articles under the principle of making available and free the research to promote the exchange of global knowledge and contribute to a greater extension, publication, evaluation and extensive use of the articles that can be used without purpose As long as reference is made to the primary source.
Conflicts of interest: authors must declare in a mandatory manner the presence or not of conflicts of interest in relation to the investigation presented.
(Download Statement of potential conflicts of interest)
The Revista Archivo Médico de Camagüey is under a License Creative Commons Attribution-Noncommercial-No Derivative Works 4.0 International (CC BY 4.0).
This license allows others to distribute, to mix, to adjust and to build from its work, even for commercial purposes, as long as it is recognized the authorship of the original creation. This is the most helpful license offered. Recommended for maximum dissemination and use of licensed materials. The full license can be found at: https://creativecommons.org/licenses/












 22 julio 2025
22 julio 2025