Characterization of clinical and laboratory behavior of patients with suspected dengue
Abstract
Background: dengue is an infectious disease widespread in several regions of the planet.
Objective: to characterize the behavior of some clinical and laboratory parameters of patients with suspected dengue.
Methods: a prospective longitudinal analytical study was carried out at the Amalia Simoni Teaching Surgical Clinical Hospital in the period from June 2016 to June 2017. The universe consisted of 151 patients from which a sample of simple probabilistic form composed of 90 patients was selected randomly. The data was collected in a form and processed in a database created with SPSS v23.
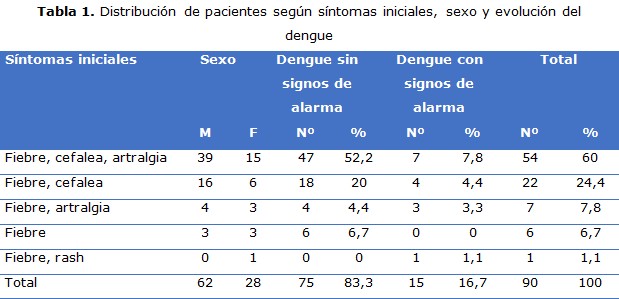
Results: the results grouped in the form of tables, showed predominance of male patients, the most frequent initial symptoms were due to fever associated with headache and arthralgia.
Conclusions: among the most frequent initial symptoms, patients with no signs of dengue alarm predominated, the appearance of these signs was significantly associated with leukocytosis, elevated hematocrit and thrombocytopenia.
DeCS: DENGUE/epidemiology; DENGUE/etiology; SIGNS AND SYMPTOMS; MANDATORY TESTING; CLINICAL LABORATORY TECHNIQUES.
Downloads
References
1. Guzmán Tirado MG, Harris E. Dengue. Lancet [Internet]. 2015 [citado 22 Abr 2019];385(9966):[aprox. 22 p.]. Disponible en: https://www.clinicalkey.es/#!/content/playContent/1-s2.0-S0140673614605729?returnurl=https:%2F%2Flinkinghub.elsevier.com%2Fretrieve%2Fpii%2FS0140673614605729%3Fshowall%3Dtrue&referrer=https:%2F%2Fwww.ncbi.nlm.nih.gov%2F
2. Tewari K, Tewari VV, Mehta R. Clinical and Hematological Profile of Patients with Dengue Fever at a Tertiary Care Hospital - An Observational Study. Mediterr J Hematol Infect Dis [Internet]. 2018 [citado 22 Mar 2019];10(1):[aprox. 11 p.]. Disponible en: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5841935/pdf/mjhid-10-1-e2018021.pdf
3. Acao Francois L, Betancourt Bethencourt JA, Gonzales Ronquillo Y. Actualización sobre fiebres hemorrágicas virales. AMC [Internet]. 2015 [citado 22 Jul 2019];19(3):[aprox. 8 p.]. Disponible en: http://scielo.sld.cu/scielo.php?script=sci_arttext&pid=S1025-02552015000300011&lng=es
4. León Ramentol CC, Betancourt Bethencourt JA, Nicolau Pestana E, Torres Tellez K. Biomarcadores para la predicción de la gravedad del dengue. CCM [Internet]. Abr-Jun 2016 [citado 27 Mar 2019];20(2):[aprox. 5 p.]. Disponible en: http://scielo.sld.cu/scielo.php?script=sci_arttext&pid=S1560-43812016000200008&nrm=iso
5. Kitab B, Kohara M, Tsukiyama-Kohara K. Experimental in vitro and in vivo systems for studying the innate immune response during dengue virus infections. Arch Virol [Internet]. 2018 [citado 27 Mar 2019];163(7):[aprox. 10 p.]. Disponible en: https://link.springer.com/content/pdf/10.1007%2Fs00705-018-3784-z.pdf
6. Linero Terán AS, María Velasco M, Chan Guevara L, Guerra Terán G. Anterior clasificación del dengue y nueva propuesta de a OMS. Concordancia en el requerimiento de hospitalización en un grupo de pacientes pediátricos hospitalizados. Rev Colomb Salud Libre [Internet]. 2015 [citado 27 Mar 2019];5(1):[aprox. 8 p.]. Disponible en:
http://revistasojs.unilibrecali.edu.co/index.php/rcslibre/article/download/174/202
7. Nunes AR, Alves BE, Pereira HW, Nascimento YM, Morais IC, Fernandes JV, et al. Improved reverse transcription-polymerase chain reaction assay for the detection of flaviviruses with semi-nested primers for discrimination between dengue virus serotypes and Zika virus. Mem Inst Oswaldo Cruz [Internet]. 2018 [citado 27 Mar 2019];113(5):[aprox.6 p.]. Disponible en:
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5853760/pdf/0074-0276-mioc-113-5-e170393.pdf
8. Bodinayake CK, Tillekeratne LG, Nagahawatte A, Devasiri V, Kodikara Arachchi W, Strouse JJ, et al. Evaluation of the WHO 2009 classification for diagnosis of acute dengue in a large cohort of adults and children in Sri Lanka during a dengue-1 epidemic. PLoS Negl Trop Dis [Internet]. 2018 [citado 27 Mar 2019];12(2):[aprox. 11 p.]. Disponible en:
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5823472/.
9. Huang WC, Lee IK, Chen YC, Tsai CY, Liu JW. Characteristics and predictors for gastrointestinal hemorrhage among adult patients with dengue virus infection: Emphasizing the impact of existing comorbid disease(s). PLoS One [Internet]. 2018 [citado 27 Mar 2019];13(2):[aprox.10 p.]. Disponible en:
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5819790/.
10. Abdi S, Wadugodapitiya A, Bedaf S, George CE, Norman G, Hawley M, et al. Identification of priority health conditions for field-based screening in urban slums in Bangalore, India. BMC Public Health [Internet]. 2018 [citado 27 Mar 2019];18(1):[aprox. 15 p.]. Disponible en:
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5833095/.
11. Mishra N, Caciula A, Price A, Thakkar R, Ng J, Chauhan LV, et al. Diagnosis of Zika Virus Infection by Peptide Array and Enzyme-Linked Immunosorbent Assay. mBio [Internet]. 2018 [citado 27 Mar 2019];9(2):[aprox. 9 p.]. Disponible en: http://mbio.asm.org/content/9/2/e00095-18.full.pdf
12. Gui L, Zhang Q, Cai Y, Deng X, Zhang Y, Li C, et al. Effects of let-7e on LPS-Stimulated THP-1 Cells Assessed by iTRAQ Proteomic Analysis. Proteomics Clin Appl [Internet]. 2018 [citado 27 Mar 2019];12(5):[aprox. 5 p.]. Disponible en:
https://onlinelibrary.wiley.com/doi/pdf/10.1002/prca.201700012
13. Thomas S, Verma J, Woolfit M, O'Neill SL. Wolbachia-mediated virus blocking in mosquito cells is dependent on XRN1-mediated viral RNA degradation and influenced by viral replication rate. PLoS Pathog [Internet]. 2018 [citado 27 Mar 2019];14(3):[aprox. 7 p.]. Disponible en:
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5833283/.
14. Rodríguez Salazar CA, Recalde Reyes DP, González MM, Padilla Sanabria L, Quintero Álvarez L, Gallego Gómez JC, et al. Manifestaciones clínicas y hallazgos de laboratorio de una serie de casos febriles agudos con diagnóstico presuntivo de infección por el virus dengue. Quindío (Colombia). Infect [Internet]. 2016 [citado 27 Mar 2019];20(2):[aprox.9 p.]. Disponible en:
http://www.scielo.org.co/scielo.php?script=sci_arttext&pid=S0123-93922016000200005&nrm=iso
15. Htun HL, Yeo TW, Tam CC, Pang J, Leo YS, Lye DC. Metformin Use and Severe Dengue in Diabetic Adults. Sci Rep [Internet]. 2018 [citado 27 Mar 2019];8(1):[aprox. 9 p.]. Disponible en:
https://www.nature.com/articles/s41598-018-21612-6.pdf
16. Gupta BP, Tuladhar R, Kurmi R, Manandhar KD. Dengue periodic outbreaks and epidemiological trends in Nepal. Ann Clin Microbiol Antimicrob [Internet]. 2018 [citado 27 Mar 2019];17(1):[aprox.6 p.]. Disponible en:
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5824540/pdf/12941_2018_Article_258.pdf
17. Suwarto S, Hidayat MJ, Widjaya B. Dengue score as a diagnostic predictor for pleural effusion and/or ascites: external validation and clinical application. BMC Infect Dis [Internet]. 2018 [citado 27 Mar 2019];18(1):[aprox. 11 p.]. Disponible en: https://bmcinfectdis.biomedcentral.com/track/pdf/10.1186/s12879-018-2996-x?site=bmcinfectdis.biomedcentral.com
18. Rojas Jaimes J, Ramos Castillo J. Características de los exámenes de laboratorio en pacientes con dengue grave en un Hospital de Puerto Maldonado-Perú. An Fac med [Internet]. 2014 [citado 27 Mar 2019];75(3):[aprox. 8 p.]. Disponible en: http://www.scielo.org.pe/scielo.php?script=sci_arttext&pid=S1025-55832014000300008
19. Lugo S, Morilla L, Bejarano O, Basualdo W, Pavlicich V. Dengue con signos de alarma ¿Podemos predecir evolución a grave desde la emergencia? Rev Bol Ped [Internet]. 2015 [citado 19 Nov 2019];54(1):25-32. Disponible en: http://www.scielo.org.bo/scielo.php?script=sci_arttext&pid=S1024-06752015000100007&lng=es
20. Gonzalez Duran E, Vazquez Pichardo M, Torres Flores JM, Garces Ayala F, Mendez Tenorio A, Curiel Quesada E, et al. Genotypic variability analysis of DENV-1 in Mexico reveals the presence of a novel Mexican lineage. Arch Virol [Internet]. 2018 [citado 27 Mar 2019];163(6):[aprox. 5 p.]. Disponible en:
https://link.springer.com/content/pdf/10.1007%2Fs00705-018-3759-0.pdf
21. Mallhi TH, Khan AH, Adnan AS, Sarriff A, Khan YH, Gan SH. Short-term renal outcomes following acute kidney injury among dengue patients: A follow-up analysis from large prospective cohort. PLoS One [Internet]. 2018 [citado 27 Mar 2019];13(2):[aprox. 8 p.]. Disponible en:
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5826532/.
22. Frantchez V, Fornelli R, Sartori GP, Arteta Z, Cabrera S, Sosa L, et al. Dengue en adultos: diagnóstico, tratamiento y abordaje de situaciones especiales. Rev Méd Urug [Internet]. 2016 [citado 27 Mar 2019];32(1):[aprox.10 p.]. Disponible en:
http://www.scielo.edu.uy/scielo.php?script=sci_arttext&pid=S1688-03902016000100006&nrm=iso
23. Céspedes Lesczinsky M, Díez M, Tobías F, Tereba I. Dengue: manifestaciones clínicas y de laboratorios más frecuentes durante las epidemias 2011-2012 en Trinidad - Bolivia. Rev Bol Ped [Internet]. 2015 [citado 27 Mar 2019];54(1):[aprox. 10 p.]. Disponible en:
http://www.scielo.org.bo/scielo.php?script=sci_arttext&pid=S1024-06752015000100002&nrm=iso
24. Fleitas Mendoza E, Ortiz Ovelar C, Ferreira Gaona M, Díaz Reissner C. Caracterización epidemiológica del dengue en la Unidad de Terapia Intensiva Adultos. Hospital Central Dr. Emilio Cubas del Instituto de Previsión Social, Paraguay. Mem Inst Investig Cienc Salud [Internet]. 2015 [citado 27 Mar 2019];13(1):[aprox.6 p.]. Disponible en:
http://scielo.iics.una.py/scielo.php?script=sci_arttext&pid=S1812-95282015000100006&nrm=iso
25. Alvarado Castro VM, Ramírez Hernández E, Paredes Solís S, Legorreta Soberanis J, Saldaña Herrera VG, Salas Franco LS, et al. Caracterización clínica del dengue y variables predictoras de gravedad en pacientes pediátricos en un hospital de segundo nivel en Chilpancingo, Guerrero, México: serie de casos. Bol Med Hosp Infant Mex [Internet]. 2016 [citado 11 Oct 2019];73(4):[aprox. 6 p.]. Disponible en: http://www.scielo.org.mx/scielo.php?script=sci_arttext&pid=S1665-11462016000400237&lng=es
26. Araya Umaña LC, Wilson Salazar E. Dengue: hallazgos hematológicos y de imagen. Rev Méd Costa Rica Centroam [Internet]. 2016 [citado 27 Mar 2019];73(620):[aprox. 4 p.]. Disponible en:
http://www.medigraphic.com/pdfs/revmedcoscen/rmc-2016/rmc163at.pdf
Published
How to Cite
Issue
Section
License
Copyright (c) 2020 Teresa Martín-Hernández, Cira Cecilia León-Ramentol, José Aureliano Betancourt-Bethencourt, Alexis Culay-Pérez, Lidyce Quesada-Leyva, Norberto Juan Nápoles-Jímenez

This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License.
Copyright: Camagüey Medical Archive Magazine, offers immediately after being indexed in the SciELO Project; Open access to the full text of the articles under the principle of making available and free the research to promote the exchange of global knowledge and contribute to a greater extension, publication, evaluation and extensive use of the articles that can be used without purpose As long as reference is made to the primary source.
Conflicts of interest: authors must declare in a mandatory manner the presence or not of conflicts of interest in relation to the investigation presented.
(Download Statement of potential conflicts of interest)
The Revista Archivo Médico de Camagüey is under a License Creative Commons Attribution-Noncommercial-No Derivative Works 4.0 International (CC BY 4.0).
This license allows others to distribute, to mix, to adjust and to build from its work, even for commercial purposes, as long as it is recognized the authorship of the original creation. This is the most helpful license offered. Recommended for maximum dissemination and use of licensed materials. The full license can be found at: https://creativecommons.org/licenses/












 22 julio 2025
22 julio 2025