Associated factors with the development of the bronchiolitis
Abstract
Background: the acute bronchiolitis is a disease caused by viruses that produced obstruction of the airways in children less than two years old.
Objective: to determine the factors associated with the development of acute bronchiolitis.
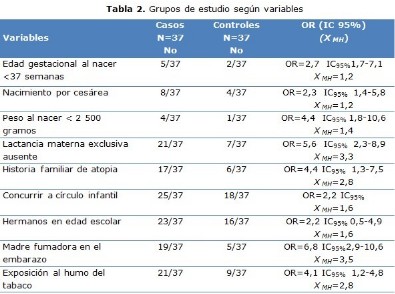
Methods: a case-control study was made in Guáimaro, Camagüey province, Cuba from June 2015 to January 2017. The cases were 37 children under two years old with diagnostic of bronchiolitis and the same number of children without diagnostic were the controls. The information was obtained through a questionnaire applied to parents of children. The variables analyzed were age, gender, severity, weight at birth, gestational age at birth, childbirth, breastfeeding, family history of atopic disease, siblings in scholar age, nursery assistance, smoker mother during pregnancy and exposition to tobacco smoke in the home.
Results: there was predominance of the minors of six months, of masculine sex and classified of light. There was significant relationships between bronchiolitis and the smoker mother during pregnancy, absence of exclusive breastfeeding, family history of atopic disease and exposition to tobacco smoke in the home.
Conclusions: were factors for the development of bronchiolitis: mother smoked during pregnancy, absence of exclusive breastfeeding, family history of atopic disease and exposition to tobacco smoke in the home.
DeCS: BRONCHIOLITIS, VIRAL/diagnosis; INFANT; RISK FACTORS; CASE-CONTROL STUDIES; AIRWAY OBSTRUCTION/etiology.
Downloads
References
1. García Meriño A, Mora Gandarillas I. Bronquiolitis aguda: diagnóstico y tratamiento. FAPap Monogr [Internet]. 2015 [citado 12 Sep 2019];1(1):[aprox. 9 p.]. Disponible en: https://monograficos.fapap.es/articulo/10/bronquiolitis-aguda-diagnostico-y-tratamiento
2. Alvarez Arzuaga D, Aguilar Perez C, Sánchez Moreno B, Tamayo Zamora M, Cumbrera Castillo B. Costos hospitalarios en pacientes con bronquiolitis. Julio–Octubre, 2015. MULTIMED [Internet]. 2017 [citado 12 Sep 2019];21(5):[aprox. 16 p.]. Disponible en: http://www.revmultimed.sld.cu/index.php/mtm/article/view/613
3. Ramos Fernández JM, Pedrero Segura E, Gutiérrez Bedmar M, Delgado Martín B, Cordón Martínez AM, Moreno Pérez D, et al. Epidemiología de los ingresos por bronquiolitis en el sur de Europa: análisis de las epidemias 2010-2015. An Pediatr (Barc) [Internet]. 2017 [citado 12 Sep 2019];87(5):[aprox. 9 p.]. Disponible en: https://www.sciencedirect.com/science/article/pii/S1695403316302740
4. Ingelfinger JR, Meissner HC. Viral Bronchiolitis in Children. N Engl J Med [Internet]. 2016 [citado 12 Sep 2019];374(1):[aprox. 11 p.]. Disponible en: https://pngpaediatricsociety.org/wp-content/uploads/2015/12/Meissner-HC-Viral-bronchiolitis-in-children-NEJM-2015.pdf
5. Callén Blecua M, Praena Crespo M, García Merino A, Mora Gandarillas I. Bronquiolitis. Diagnóstico y tratamiento en Atención Primaria [Internet]. España: Grupo de Vías Respiratorias de la Asociación Española de Pediatría de Atención Primaria; 2015 [citado 12 Sep 2019]. Disponible en: http://www.respirar.org/images/pdf/grupovias/bronquiolitis_p_gvr_4_2015.pdf
6. Martínez García L, Pardo Hernández H, Alonso-Coello P. ¿Es urgente actualizar las guías de práctica clínica españolas para el tratamiento de la bronquiolitis aguda? An Pediatr (Barc) [Internet]. 2016 [citado 20 Jun 2018];85(2):[aprox. 3 p.]. Disponible en: https://www.analesdepediatria.org/index.php?p=revista&tipo=pdf-simple&pii=S1695403316000229
7. Oñate Ramírez AL, Rendón Macías ME, Iglesias Leboreiro J, Bernárdez Zapata I. Apego a guías clínicas para el manejo de bronquiolitis. Bol Med Hosp Infant Mex [Internet]. Ago 2014 [citado 20 Jun 2018];71(4):[aprox. 7 p.]. Disponible en: http://www.scielo.org.mx/scielo.php?script=sci_arttext&pid=S1665-11462014000400006&lng=es
8. McConnochie KM. Bronchiolitis. What’s in the name? Am J Dis Child [Internet]. 1983 [citado 20 Jun 2018];137(1):[aprox. 7 p.]. Disponible en: https://www.researchgate.net/publication/16350972_Bronchiolitis_What's_in_the_Name
9. Wood DW, Downes JJ, Lecks HI. A clinical scoring system for the diagnosis of respiratory failure. Preliminary report on childhood status asthmaticus. Am J Dis Child. 1972;123(3):227-8.
10. Pinchak C, Schelotto M, Borges P, Zunino V, Cuturi B, Izuibejeres C, et al . Modificaciones en el tratamiento de pacientes con bronquiolitis luego de la radiografía de tórax. Arch Pediatr Urug [Internet]. Ago 2017 [citado 12 Jun 2018];88(4):[aprox. 10 p.]. Disponible en: http://www.scielo.edu.uy/scielo.php?script=sci_arttext&pid=S1688-12492017000400189&lng=pt
11. Ramos-Fernández JM, Moreno-Pérez D, Gutiérrez-Bedmar M, Hernández-Yuste A, Cordón-Martínez AM, Milano-Manso G, et al. Predicción de la evolución de la bronquiolitis por virus respiratorio sincitial en lactantes menores de 6 meses. Rev Esp Salud Pública [Internet]. 2017 [citado 12 Jun 2018];91:[aprox. 6 p.]. Disponible en: http://www.scielosp.org/scielo.php?script=sci_arttext&pid=S1135-57272017000100401&lng=pt
12. Muñoz-Quiles C, López-Lacort M, Úbeda-Sansano I, Alemán-Sánchez S, Pérez-Vilar S, Puig-Barber? J, et al. Population based analysis of bronchiolitis epidemiology in Valencia, Spain. Pediatr Infect Dis J [Internet]. 2016 [citado 12 Sep 2019];35:[aprox. 6 p.]. Disponible en: http://dx.doi.org/10.1097/INF.0000000000000993
13. Bayona Ovalles Y, Niederbacher Velásquez J. Infecciones respiratorias virales en pediatría: generalidades sobre fisiopatogenia, diagnóstico y algunos desenlaces clínicos. Medicas UIS [Internet]. Abr 2015 [citado 12 Sep 2019];28(1):[aprox. 5 p.]. Disponible en: http://www.scielo.org.co/scielo. php?script=sci_arttext&pid=S0121-03192015000100014&lng=pt
14. Golan‐Tripto I, Goldbart A, Akel K, Dizitzer Y, Novack V, Tal A. Modified Tal Score: Validated score for prediction of bronchiolitis severity. Pediatric Pulmonol. 2018;53(6):796-801.
15. Cano Fernández J, Zabaleta Camino C, De la Torre Montes de Neira E, Chullen Y, Melendi Crespo JM, Sánchez Bayle M. Tabaquismo pasivo prenatal y posnatal y bronquiolitis. An Pediatr (Barc). 2003;58:115-20.
16. Vitor Gavidia GC. Lactancia materna no exclusiva como factor de riesgo de bronquiolitis en menores de 2 años Hospital General María Auxiliadora 2017 [tesis]. Lima, Perú: Universidad Privada San Juan Bautista; 2018 [citado 26 Jun 2018]. Disponible en: http://repositorio.upsjb.edu.pe/bitstream/handle/upsjb/1523/T-TPMC-%20Gabriela%20Carolina%20%20Vitor%20Gavidia.pdf?sequence=1&isAllowed=y
17. Ayuso Raya C, Castillo Serrano A, Escobar Rabadán F, Plaza Almeida J. Bronquiolitis en una Zona de Salud urbana: Factores demográficos y medioambientales. Rev Clín Med Fam. 2010;3(2):71-7.
18. Martins M, Pereira N, Reis R, Tomaz E. Risk factors for recurrent wheezing after the first hospitalization for bronchiolitis. Rev Port Imunoalergol. 2015;23(4):223-30.
19. Aguilar Cordero MJ, Baena García L, Sánchez López AM, Guisado Barrilao R, Hermoso Rodríguez E, Mur Villar N. Beneficios inmunológicos de la leche humana para la madre y el niño. Revisión sistemática. Nutr Hosp. 2016;33:482-93.
20. Ruiz Silva M, Hernández Pérez I, Montes de Oca Domínguez M. Comportamiento clínico-epidemiológico de la bronquiolitis aguda en lactantes admitidos. Belmopán, Belice. 2015. MULTIMED [Internet]. 2017 [citado 26 Jun 2018];21(3):[aprox. 15 p.]. Disponible en: http://www.revmultimed.sld.cu/index.php/mtm/article/view/534
21. Martín Martín R, Sánchez Bayle M. Tabaquismo pasivo en la infancia y patología respiratoria de las vías bajas en una consulta de Atención Primaria. Rev Pediatr Aten Primaria [Internet]. Dic 2009 [citado 12 Sep 2019];11(44):[aprox. 9 p.]. Disponible en: http://scielo.isciii.es/scielo.php? script=sciarttext&pid=S1139-76322009000500004&lng=es
22. Marco Tejero A, Pérez Trullén A, Córdoba García R, García Sánchez N, Cabañas Bravo MJ. La exposición al humo de tabaco en el hogar aumenta la frecuentación por patología respiratoria en la infancia. An Pediatr (Barc). 2007;66(5):475-80.
Published
How to Cite
Issue
Section
License
Copyright (c) 2019 Carlos Coronel-Carvajal

This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License.
Copyright: Camagüey Medical Archive Magazine, offers immediately after being indexed in the SciELO Project; Open access to the full text of the articles under the principle of making available and free the research to promote the exchange of global knowledge and contribute to a greater extension, publication, evaluation and extensive use of the articles that can be used without purpose As long as reference is made to the primary source.
Conflicts of interest: authors must declare in a mandatory manner the presence or not of conflicts of interest in relation to the investigation presented.
(Download Statement of potential conflicts of interest)
The Revista Archivo Médico de Camagüey is under a License Creative Commons Attribution-Noncommercial-No Derivative Works 4.0 International (CC BY 4.0).
This license allows others to distribute, to mix, to adjust and to build from its work, even for commercial purposes, as long as it is recognized the authorship of the original creation. This is the most helpful license offered. Recommended for maximum dissemination and use of licensed materials. The full license can be found at: https://creativecommons.org/licenses/












 22 julio 2025
22 julio 2025