Evaluating the fetal risk in patients diagnosed with fetal distressing status with intrauterine revival
Keywords:
estado fetal intranquilizante, reanimación intraútero efectiva, factores de riesgo.Abstract
Background: the term fetal imprecise suffering has low predictive value even in populations of high risk.
Objective: to evaluate the fetal risk in patients who underwent Cesarean sections and diagnosed with fetal distressing status with effective intrauterine revival.
Methods: a quasi-experimental accomplished study was conducted for two groups in patients diagnosed with fetal distressing status with intrauterine revival at Ana Betancourt de Mora hospital from June 1st, 2014 to February 1st, 2015.
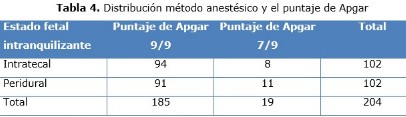
Results: the fetal distressing status was associated with effective intrauterine revival and the conditions of the umbilical cord with odss ratio 1.3. The probability of the diagnosis of fetal distressing status with intrauterine revival was 5.6 times more for patients with hypertensive disease in pregnancy. Probability was 4.3 times for diabetes. The diagnosis of fetal distressing status was not associated with effective intrauterine revival and the neuroaxial anesthesia.
Conclusions: fetal risk factors for patients who underwent Cesarean sections with the diagnosis of fetal distressing status with effective intrauterine revival were: hypertension during pregnancy, diabetes, alterations of the umbilical cord and neuroaxial anesthesia was independent of fetal risk of patients.
DeCS: FETAL DISTRESS; RISK FACTORS; CESAREAN SECTION; RISK ASSESSMENT; EPIDEMIOLOGY, EXPERIMENTAL.
Downloads
References
1. Hasegawa J, Toyokawa S, Ikenoue T, Asano Y, Satoh S, Ikeda T, et al. Relevant Obstetric Factors for Cerebral Palsy: From the Nationwide Obstetric Compensation System in Japan. Prevention Recurrence Committee, Japan Obstetric Compensation System for Cerebral Palsy. PLoS One [Internet]. 2016 Jan 28 [citado 2016 Feb 3];11(1):[about 5 p.]. Available from: http://journals.plos.org/plosone/article?id=10.1371/journal.pone.0148122
2. Jenniskens K, Janssen PA. Newborn outcomes in britishcolumbia after caesarean section for non-reassuring fetal status. J Obstet Gynaecol Can [Internet]. 2015 Mar [citado 2015 May 23];37(3):[about 6 p]. Available from: http://www.sciencedirect.com/science/article/pii/S1701216315303066
3. Groen RS, Trelles M, Caluwaerts S, Papillon-Smith J, Noor S, Qudsia B, et al. A cross-sectional study of indications for cesarean deliveries in Médecins Sans Frontières facilities across 17 countries. Int J Gynaecol Obstet. 2015 Jun;129(3):231-5.
4. La Fontaine Terry E, La Fontaine Terry JC, Paulina Simba N, Cutiño Guerra M. Morbilidad materna y neonatal en la cesárea primitiva. Arch Méd Cam [Internet]. 2006 [citado 12 Mar 2015];10(3):[aprox. 6 p.]. Disponible en: http://scielo.sld.cu/scielo.php?script=sci_arttext&pid=S1025-02552006000300003
5. Valdés Dacal S. La cesárea necesaria. Consultas Médicas. Periódico Adelante de la provincia cubana de Camagüey. 2016 Sep;Secc. Médica (Col. 2).
6. Preboth M. ACOG. Guidelines on Antepartum Fetal Surveillance. American Family Physician [Internet]. 2000 Sept 1 [citado 2014 Sep 25];62(5):[about 4 p]. Available from: http://www.aafp.org/afp/20000901/practice.htm
7. Organización Mundial de la salud. Declaracion de la OMS sobre tasas de cesáreas [Internet]. Ginebra, Suiza: Departamento de Salud Reproductiva e Investigación Organización Mundial de la Salud; 2015 [citado 4 Nov 2016]. Disponible en: www.who.int/reproductivehealth/.
8. Ye J, Zhang J, Mikolajczyk R, Torloni MR, Gülmezoglu AM, Betrán AP. Association between rates of caesarean section and maternal and neonatal mortality in the 21st century: a worldwide population-based ecological study with longitudinal data. BJOG. 2015 Aug 24 (Epub ahead of print).
9. Betran AP, Torloni MR, Zhang J, Ye J, Mikolajczyk R, Deneux-Tharaux C, et al. What is the optimal rate of caesarean section at population level? A systematicreview of ecologicstudies. Reprod Health. 2015;12(1):57.
10. Betran AP, Vindevoghel N, Souza JP, Gulmezoglu AM, Torloni MR. A Systematic Review of the Robson Classification for Caesarean Section: What Works, Doesn’t Work and How to Improve It. PLoS One. 2014;9(6):e97769.
11. Dekker GA. Management of preeclampsia. Pregnancy Hypertens [Internet]. 2014 Jul [citado 2015 Nov 26];4(3):[about 7 p.]. Available from: http://www.sciencedirect.com/science/article/pii/S2210778914000804/pdfft?md5=27ea3a3098ec0aa9731c1dfe84dba5d0&pid=1-s2.0-S2210778914000804-main.pdf
12. Ortner CM, Combrinck B, Allie S, Story D, Landau R, Cain K, et al. Strong ion and weak acid analysis in severe preeclampsia: potential clinical significance. Br J Anaesth [Internet]. 2015 Aug [citado 2015 Dec 16];115(2):[about 9 p.]. Available from: http://bja.oxfordjournals.org/content/115/2/275.long
13. Lurie S, Ribenzaft S, Boaz M, Golan A, Sadan O. The effect of cigarette smoking during pregnancy on mode of delivery in uncomplicated term singleton pregnancies. J Matern Fetal Neonatal Med [Internet]. 2014 May [citado 2015 Ene 21];27(8):[about 9 p.]. Available from: http://www.tandfonline.com/doi/pdf/10.3109/14767058.2013.842551
14. Grace L, Greer RM, Kumar S. Perinatal consequences of a category 1 caesarean section at term. BMJ Open [Internet]. 2015 [citado 2016 Ene 2];5(7):[about 4 p.]. Available from: http://www.ncbi.nlm.nih.gov/pmc/articles/PMC4521509/
15. Nishida Y, Matsumoto S, Noguchi T, Narahara H. New evaluation of fetal oxidative stress: measurement of the umbilical cord blood dimethyl sulfate-induced ascorbyl free radical by an electron spin resonance method. J Matern Fetal Neonatal Med [Internet]. 2014 [citado 2015 Ene 16];27(15):[about 6 p.]. Available from: http://www.tandfonline.com/doi/pdf/10.3109/14767058.2013.868427
16. López Stewart G. Tratamiento de la diabetes en el embarazo: ¿algo nuevo? Rev Méd Clín Condes [Internet]. Mar 2016 [citado 4 Nov 2016];27(2):[aprox. 5 p.]. Disponible en: http://dx.doi.org/10.1016/j.rmclc.2016.04.014
17. Wood S, Ross S, Sauve R. Cesarean Section and Subsequent Stillbirth, Is Confounding by Indication Responsible for the Apparent Association? An Updated Cohort Analysis of a Large Perinatal Database. PLoS One [Internet]. 2015 Sep 2 [citado 2015 Sep 26];10(9):[about 11 p.]. Available from: http://www.ncbi.nlm.nih.gov/pmc/articles/PMC4557984/.
18. Ryo E, Kamata H, Seto M. Decreased fetal movements at home were recorded by a newly developed fetal movement recorder in a case of a non-reassuring fetal status. J Matern Fetal Neonatal Med [Internet]. 2014 Oct [citado 2015 Agu 4];27(15):[about 11 p.]. Available from: http://www.tandfonline.com/doi/pdf/10.3109/14767058.2013.863868
19. Nápoles Méndez D, Piloto Padrón M. Consideraciones actuales sobre la operación cesárea. Medisan [Internet]. 2012 [citado 14 Abr 2015];16(10):[aprox. 10 p.]. Disponible en: http://www.bvs.sld.cu/revistas/san/vol_16_10_12/san131012.html€
20. Hasegawa J, Ikeda T, Sekizawa A, Ishiwata I, Kinoshita K; Japan Association of Obstetricians and Gynecologists, Tokyo, Japan. Obstetric risk factors for umbilical cord prolapse: a nationwide population-based study in Japan. Arch Gynecol Obstet [Internet]. 2016 Sep [citado 2016 Jan 7];294(3):[about 6 p.]. Available from: http://www.pubfacts.com/detail/26714678/Obstetric-risk-factors-for-umbilical-cord-prolapse-a-nationwide-population-based-study-in-Japan
21. Nishida Y, Matsumoto S, Noguchi T, Narahara H. New evaluation of fetal oxidative stress: measurement of the umbilical cord blood dimethyl sulfate-induced ascorbyl-free radical by an electron spin resonance method. J Matern Fetal Neonatal Med [Internet]. 2014 [citado 2015 Agu 4];27(15):[about 9 p.]. Available from: http://www.tandfonline.com/doi/pdf/10.3109/14767058.2013.868427
22. Figueras F, Savchev S, Triunfo S, Crovetto F, Gratacos E. An integrated model with classification criteria to predict small-for-gestational-age fetuses at risk of adverse perinatal outcome. Ultrasound Obstet Gynecol [Internet]. 2015 Mar [citado 2015 Nov 3];45(3):[about 7 p]. Available from: http://onlinelibrary.wiley.com/doi/10.1002/uog.14714/full
23. Parra-Saavedra M, Simeone S, Triunfo S, Crovetto F, Botet F, Nadal A, et al. Correlation between histological signs of placental underperfusion and perinatal morbidity in late-onset small-for-gestational-age fetuses. Ultrasound Obstet Gynecol [Internet]. 2015 Feb [citado 2015 Sep 3];45(2):[about 6 p.]. Available from: http://onlinelibrary.wiley.com/doi/10.1002/uog.13415/full
24. Catlin EA, Carpenter MW, Brann BS. The Apgar score revisited: influence of gestacional age. J Pediatr. 1986;109:865.
25. Committee on Drugs. The transfer of drugs and other chemicals into human milk. Pediatrics. 1994;93:137.
26. Committee on Fetus and Newborn. Use and abuse of the Apgar score. Pediatrics. 1986;78(1):148.
27. Costley PL, East CE. Oxytocin augmentation of labour in women with epidural analgesia for reducing operative deliveries. Cochrane Database Syst Rev [Internet]. 2012 May [citado 2015 Jan 2];16:[about 4 p.]. Available from: http://onlinelibrary.wiley.com/doi/10.1002/14651858.CD009241.pub3/full
Published
How to Cite
Issue
Section
License
Copyright (c) 2017 Zaily Fuentes Díaz, Patricia Díaz Requejo, Sarah E. López Lazo, Orlando Rodríguez Salazar

This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License.
Copyright: Camagüey Medical Archive Magazine, offers immediately after being indexed in the SciELO Project; Open access to the full text of the articles under the principle of making available and free the research to promote the exchange of global knowledge and contribute to a greater extension, publication, evaluation and extensive use of the articles that can be used without purpose As long as reference is made to the primary source.
Conflicts of interest: authors must declare in a mandatory manner the presence or not of conflicts of interest in relation to the investigation presented.
(Download Statement of potential conflicts of interest)
The Revista Archivo Médico de Camagüey is under a License Creative Commons Attribution-Noncommercial-No Derivative Works 4.0 International (CC BY 4.0).
This license allows others to distribute, to mix, to adjust and to build from its work, even for commercial purposes, as long as it is recognized the authorship of the original creation. This is the most helpful license offered. Recommended for maximum dissemination and use of licensed materials. The full license can be found at: https://creativecommons.org/licenses/












 22 julio 2025
22 julio 2025