Infections in patients with traumatic brain injury in Polytrauma Service in Camagüey from 2013 to 2015
Keywords:
Trauma craneoencefálico, infecciones nosocomiales, neumonía asociada a la ventilación.Abstract
Background: nosocomial infections or in its broadest concept hospital-acquired infections, are now one of the main problems in intensive care units. There are several factors contributing to the development of these infections in patients with traumatic brain injury, favoring the development of secondary brain injury during the post-traumatic period, correlating this event with the doubling of mortality rate.
Objective: to characterize nosocomial infections in patients with traumatic brain injury.
Methods: a descriptive transversal study was conducted in hospitalized patients in Manuel Ascunce Domenech hospital in Camagüey, from January 2013 to December 2015. The studied group was composed of 64 patients admitted and diagnosed with traumatic brain injury in which a pathogenic microorganism was isolated. Studied variables were: age groups, gender, need for artificial mechanical ventilation, discharge status, stay, isolated pathogenic microorganisms and their localizations.
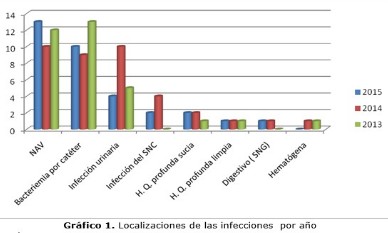
Results: the highest frequency of patients belonged to male who were between 48-57 years. Almost all of them needed artificial mechanical ventilation, and more than one third died. The stay over 21 days presented a higher frequency in patients who were hospitalized. The most frequent isolated microorganism was the acinetobacter spp, and locations of the most frequent infections were the pneumonia associated to mechanical ventilation artificially and catheter bacteremia.
Conclusions: there was a prevalence of male patients corresponding to the 48 to 57 age group. The most frequent findings were the acinetobacter spp as isolated microorganism and pneumonia associated to artificial mechanical ventilation as well as catheter bacteremia.
DeCS: CRANIOCEREBRAL TRAUMA; CROSS INFECTION; RESPIRATION, ARTIFICIAL; ACINETOBACTER; EPIDEMIOLOGY, DESCRIPTIVE.
Downloads
References
1. Ingebrigtsen T, Mortensen K, Romner B. The epidemiology of hospital-referred head injury in northern Norway. Neuroepidemiology. 1998;17(3):139-46.
2. Ramos Reyna E, Flores Vázquez J. Cuestionarios para la clasificación de pacientes con traumatismo craneoencefálico en un Servicio de Urgencias. Neurol Neurocir Psiquiat. 2011;44(1):6-12.
3. Becker DP. Head injury. En: Cecil. Textbook of medicine. 18th ed. Philadelphia: WB Saunders Company; 1988. P.2239-2244.
4. Singer M, Deutschman CS, Seymour CW, Shankar-Hari M, Annane D, Bauer M. The Third International Consensus Definitions for Sepsis and Septic Shock (Sepsis 3). JAMA [Internet]. Feb 2016 [citado 16 Jul 2016];315(8):[aprox. 14 p.]. Disponible en: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4968574/.
5. Hodelín Tablada R. Pacientes en estado vegetativo persistente o estado de mínima conciencia secundarios a traumatismos craneoencefálicos. Mediciego [Internet]. 2010 [citado 15 Feb 2017];16(1):[aprox. 8 p.]. Disponible en: http://bvs.sld.cu/revistas/mciego/vol16_supl1_10/pdf/t20.pdf
6. Kelso ML, Gendelman HE. Bridge between neuroimmunity and traumatic brain injury. Curr Pharm Des [Internet]. 2014 [citado 15 Feb 2017];20(26):[about 14 p.]. Available from: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4135046
7. The ARISE investigators and the ANZICS Clinical Trials Group. Goal-Directed Resuscitation for patients with early Septic Shock. N Engl J Med [Internet]. 2014 Oct 16 [citado 2017 Feb 15];371(16):[about 12 p.]. Available from: http://www.nejm.org/doi/full/10.1056/NEJMoa1404380SO
8. The Process Investigators. A randomized Trial of Protocol-Based care for patients with early Septic Shock. N Engl J Med [Internet]. 2014 May 1 [citado 2017 Feb 15];370(18):[about 11 p.]. Available from: http://www.nejm.org/doi/full/10.1056/NEJMoa1401602SO
9. Levy MM, Rhodes A, Phillips GS, Townsend SR, Schorr CA, Beale R, et al. Surviving Sepsis Campaign: Association Between Performance Metrics and Outcomes in a 7.5-Year Study. Crit Care Med. 2015 Jan;43(1):3-12.
10. Unidades de Cuidados Intensivos (Proyecto DINUCIs) GD. Incidencia de infección relacionada con el cuidado sanitario en unidades de cuidados intensivos en Cuba. Invest medicoquir [Internet]. 2013 [citado 15 Feb 2017];5(1):[aprox. 20 p.]. Disponible en: http://www.revcimeq.sld.cu/index.php/imq/article/view/208
11. Abdo Cuza A, Castellanos Gutiérrez R, González Aguilera JC, Reyes Tornés R, Vázquez Belizón Y, Somoza García ME, et al. Incidencia y consecuencias de la traqueobronquitis asociada a ventilación mecánica en unidades de cuidados intensivos. Rev cubana med [Internet]. Mar 2013 [citado 15 Feb 2017];52(1):[aprox. 10 p.]. Disponible en: http://scielo.sld.cu/scielo.php?script=sci_arttext&pid=S0034-75232013000100003&lng=es
12. Abdo Cuza A, Castellanos Gutiérrez R. Disminución de la Infección Nosocomial en Unidades de Cuidados Intensivos y Ia Incidencia de infección relacionada con el cuidado sanitario en unidades de cuidados intensivos en Cuba. Año 2012. Invest Medicoquir [Internet]. 2013 [citado 15 Feb 2017];5(2):[aprox. 15 p.]. Disponible en: http://www.revcimeq.sld.cu/index.php/imq/article/view/237
13. Proyecto Disminución de la Infección Nosocomial en Unidades de Cuidados Intensivos G. Incidencia de infección relacionada con el cuidado sanitario en unidades de cuidados intensivos en Cuba (año 2014). Resultados de la implementación de un paquete de medidas profilácticas. Invest Medicoquir [Internet]. 2016 [citado 15 Feb 2017];7(2):[aprox. 20 p.]. Disponible en: http://www.revcimeq.sld.cu/index.php/imq/article/view/319
14. Vicent J, Bihari D, Suter P. The prevalence of nosocomial infection in intensive care units in Europe: Results of the European prevalence of infection in intensive care (EPIC) study. JAMA. 1995 Ago 23;274:639-44.
15. Zarb P, Coignard B, Griskeviciene J, Muller A, Vankerckhoven V, Weist K, et al. National Contact Points for the ECDC pilot prevalence survey of healthcare-associated infections and antimicrobial use. Euro Surveill. 2012 Nov 15;17(46):34-42.
16. Ponce de León Rosales SP, Molinar Ramos F, Domínguez-Cherit G, Rangel Frausto MS, Vázquez Ramos VG. Prevalence of infections in intensive care units in Mexico: A multicenter study. Crit Care Med. 2000 May;28(5):1316-21.
17. Grupo de trabajo de Enfermedades Infecciosas y Sepsis. Estudio Nacional de Vigilancia de Infección Nosocomial en Servicios de Medicina Intensiva (ENVIN). Informe 2014 [Internet]. España: Sociedad Española de Medicina Intensiva Critica y Unidades Coronarias; Mar 2015 [citado 16 Jul 2016]. Disponible en: http://hws.vhebron.net/envin-helics/Help/Informe%20ENVIN-UCI%202014.pdf
18. Agodi A, Auxilia F, Barchitta M, Brusaferro S, D'Alessandro D, Grillo OC, et al. Trends, risk Factors and outcomes of healthcare-associated infections within the Italian Network SPI-UTI. J Hospital Infection. 2013 May;84(1):52-8.
19. Ortiz G, Fonseca Ruiz N, Molina F, Garay M, Lara A, Dueñas C, et al. Epidemiologia de la Neumonía asociada a ventilador en 39 unidades de cuidados intensivos en Colombia (2007-2009). Informe año 2010. Acta Col Cuid Int [Internet]. 2011 [citado 15 Feb 2017];11(1):[aprox. 7 p.]. Disponible en: https://www.researchgate.net/publication/275659788
20. García Montero A. Neumonía por Acinetobacter baumannii asociada a la ventilación mecánica. Rev Cuba Med Int Emerg [Internet]. 2015 [citado 2017 Feb 15];15(1):[aprox. 10 p.]. Disponible en: http://www.revmie.sld.cu/index.php/mie/article/view/134
21. Custardoy J, Ibañez Cuerda D, Martínez Galceran J, García Pachón E. Neumonía nosocomial en el enfermo neurológico [Internet]. España: Hospital Vega Baja. Orihuela. Alicante; 1998 [citado 15 Feb 2017]. Disponible en: http://www.uninet.edu/neurocon/congreso-1/conferencias/h-general-7.html
22. Lisboa T, Rello J. Prevención de infecciones nosocomiales: estrategias para mejorar la seguridad de los pacientes en la Unidad de Cuidados Intensivos. Med Intensiva [Internet]. Jul 2008 [citado 15 Feb 2017];32(5):[aprox. 5 p.]. Disponible en: http://scielo.isciii.es/scielo.php?script=sci_arttext&pid=S0210-56912008000500006&lng=es
23. Young Lee J, Soo Ko K. Antimicrobial Resistance and Clones of Acinetobacter Species and Pseudomonas aeruginosa. J Bacteriol Virol [Internet]. Mar 2012 [citado 15 Feb 2017];42(1):[aprox. 8 p.]. Disponible en: https://synapse.koreamed.org/DOIx.php?id=10.4167/jbv.2012.42.1.1&vmode=PUBREADER
24. Vigilancia, prevención y control de las infecciones nosocomiales en los hospitales españoles. Situación actual y perspectivas. España: Informe de la Sociedad Española de Medicina Preventiva, Salud Pública e Higiene; 2002.
25. Ramírez Sandoval M, Aranza Aguilar J, Varela Ramírez M, García González A, Vélez Castro G, Salcedo Romero R, et al. Brote de infección nosocomial de vías respiratorias bajas por Acinetobacter baumannii en un servicio de Medicina Interna de un hospital general de la Ciudad de México. Med Int Mex [Internet] 2013 [citado 15 Feb 2017];29:[aprox. 6 p.]. Disponible en: https://www.cmim.org/boletin/pdf2013/MedIntContenido03_05.pdf
26. Sunenshine RH, Wright MO, Maragakis LL, Harris AD, Song X, Hebden J, et al. Multidrug-resistant Acinetobacter infection mortality rate and length of hospitalization. Emerg Infect Dis [Internet]. 2007 Ene 1[citado 2017 Feb 15];13:[about 7 p.]. Available from: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2725827/.
27. Medell Gago M, Hart Casares M, Mora Diaz I. Acinetobacter baumannii versus Pseudomonas aeruginosa. Comportamiento en pacientes críticos con ventilación mecánica. Rev cubana med [Internet]. Sep 2012 [citado 16 Feb 2017];51(3):[aprox. 7 p.]. Disponible en: http://scielo.sld.cu/scielo.php?script=sci_arttext&pid=S0034-75232012000300005&lng=es
28. Pérez Morales L, Barletta Castillo J, Quintana Hernández H, Reyes Rodríguez I, Otero Espino N. Estudio clínico, epidemiológico y microbiológico de pacientes con neumonía asociada a la ventilación mecánica ingresados en salas de cuidados intensivos. Medisur [Internet]. Ago 2012 [citado 16 Feb 2017];10(4):[aprox. 10 p.]. Disponible en: http://scielo.sld.cu/scielo.php?script=sci_arttext&pid=S1727-897X2012000400001&lng=es
29. Rodríguez Llerena B, Iraola Ferrer M, Molina Díaz F, Pereira Valdés E. Infección hospitalaria en la Unidad de Cuidados Intensivos Polivalente de un hospital universitario cubano. Rev Cubana Invest Bioméd [Internet]. Sep 2006 [citado 16 Feb 2017];25(3):[aprox. 5 p.]. Disponible en: http://scielo.sld.cu/scielo.php?script=sci_arttext&pid=S0864-03002006000300003&lng=es
Published
How to Cite
Issue
Section
License
Copyright (c) 2017 alexis culay perez, Ismael J. Ferrer Tan, Esteban Álvarez Serrano, Aymara Fernández Carmenates, Ismael M. Ferrer Herrera, Xiomara Borrego Lastre

This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License.
Copyright: Camagüey Medical Archive Magazine, offers immediately after being indexed in the SciELO Project; Open access to the full text of the articles under the principle of making available and free the research to promote the exchange of global knowledge and contribute to a greater extension, publication, evaluation and extensive use of the articles that can be used without purpose As long as reference is made to the primary source.
Conflicts of interest: authors must declare in a mandatory manner the presence or not of conflicts of interest in relation to the investigation presented.
(Download Statement of potential conflicts of interest)
The Revista Archivo Médico de Camagüey is under a License Creative Commons Attribution-Noncommercial-No Derivative Works 4.0 International (CC BY 4.0).
This license allows others to distribute, to mix, to adjust and to build from its work, even for commercial purposes, as long as it is recognized the authorship of the original creation. This is the most helpful license offered. Recommended for maximum dissemination and use of licensed materials. The full license can be found at: https://creativecommons.org/licenses/












 22 julio 2025
22 julio 2025