Actualidad en fístula pancreática postoperatoria
Resumen
Fundamento: el cáncer de páncreas presenta una alta mortalidad, producto que la mayoría de las veces se diagnóstica en etapa avanzada. El tratamiento de elección es la resección quirúrgica, la cual debida a su complejidad está acompañada de una morbimortalidad importante, cuando no se realiza en centros de alto volumen. Dentro de las complicaciones, la fístula pancreática postoperatoria, es de aparición frecuente.
Objetivo: realizar una revisión sistemática actualizada acerca del concepto y clasificación de la fístula pancreática postoperatoria.
Métodos: se realizó una revisión sistemática de la literatura con la base de datos SCOPUS bajo los criterios que establecen sus revisores, se utillizaron las siguientes palabras claves: pancreatic fistula, pancreatic surgery, complications, mortality, Whipple procedure. Se incluyeron todas las publicaciones en inglés y español. El método de análisis y síntesis se utilizó para la interpretación de la bibliografía.
Desarrollo: se revisaron 175 artículos, de los cuales, se escogieron 55, que cumplían con los criterios de selección. Entre ellos, cuatro metanálisis, ocho artículos de revisión y 33 artículos originales.
Conclusiones: el concepto y clasificación de la fístula pancreática postoperatoria constituye una herramienta válida para la comparación de resultados quirúrgicos entre instituciones. La centralización de la atención en centros de alto volumen constituye la principal medida para disminuir esta complicación.
DeCS: FÍSTULA PANCREÁTICA/cirugía; COMPLICACIONES POSOPERATORIAS; NEOPLASIAS PANCREÁTICAS/diagnóstico; NEOPLASIAS PANCREÁTICAS/mortalidad; MÁRGENES DE ESCISIÓN.
Referencias
Pila Pérez R, Vázquez García R, Pila Peláez R, Morales Morales M, Holguín Priet V. Cáncer de páncreas en Camagüey. Arch Med Camagüey [Internet]. Abr 2005 [citado 2019 Mar 05];9(2):[aprox. 14 p.]. Disponible en: http://scielo.sld.cu/sc ielo.php?script=sci_arttext&pid=S1025-0255 2005 000 200 00 6 &l ng=es
González González JL, Menéndez Núñez J, Copo Jorge JA, González Villalonga JA, Pérez García K. Resultados del tratamiento de 215 tumores pancreáticos y periampulares en el Hospital "Hermanos Ameijeiras". Rev cubana Cir [Internet]. Jun 2014 [citado 19 Ago 2018];53(2):[aprox. 11 p.]. Disponible en: http://scielo.sld.cu/scielo.php?script=sci_arttext&pid=S0034-74932014000200002
Ministerio de Salud Pública. Dirección Nacional de Estadísticas y Registros Médicos. Anuario Estadístico de Salud 2017. La Habana: MINSAP; 2018.
Nakayama Y, Konishi M, Gotohda N, Kato Y, Aizawa H, Kudo M, et al. Comparison of postoperative early and late complications between pancreas-sparing duodenectomy and pancreatoduodenectomy. Surg Today. 2017;47(6):705-11.
Iyoob VA. Prospective study of short-term complications following pancreatoduodenectomy based on international definitions. Trop Gastroenterol. 2014;35(1):32-8.
Sanford DE, Woolsey CA, Hall BL, Linehan DC, Hawkins WG, Fields RC, et al. Variations in definition and method of retrieval of complications influence outcomes statistics after pancreatoduodenectomy: comparison of NSQIP with non-NSQIP methods. J Am Coll Surg. 2014;219(3):407-15.
Stepan EV, Ermolov AS, Rogal ML, Teterin YS. [External pancreatic fistulas management]. Khirurgiia (Mosk). 2017;(3):42-9.
Bekaii Saab T. Highlights in pancreatic cancer from the 2018 American Society of Clinical Oncology Gastrointestinal Cancers Symposium: commentary. Clin Adv Hematol Oncol. 2018;16 Suppl 7(3):16-8.
Masiak Segit W, Rawicz Pruszynski K, Skorzewska M, Polkowski WP. Surgical treatment of pancreatic cancer. Pol Przegl Chir. 2018;90(2):45-53.
van Rijssen LB, Zwart MJ, van Dieren S, de Rooij T, Bonsing BA, Bosscha K, et al. Variation in hospital mortality after pancreatoduodenectomy is related to failure to rescue rather than major complications: a nationwide audit. HPB (Oxford). 2018;20(8):759-67.
Mohammed S, Fisher WE. Quality metrics in pancreatic surgery. Surg Clin North Am. 2013;93(3):693-709.
Levy MJ, Chari S, Adler DG, Clain JE, Gostout CJ, Harewood GC, et al. Complications of temporary pancreatic stent insertion for pancreaticojejunal anastomosis during pancreaticoduodenectomy. Gastrointest Endosc. 2004;59(6):719-24.
Waugh CE. Pancreatogastroanastomosis en pancreatoduodenectomía. Una alternativa segura de anastomosis al muñón pancreático. Rev Chil Cir. 2002;54(1):59-64.
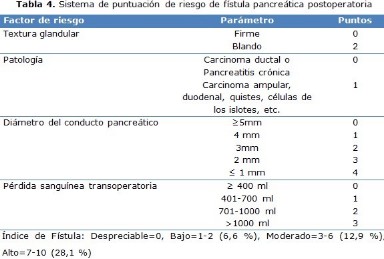
Pratt WB, Callery MP, Vollmer CM. Risk prediction for development of pancreatic fistula using the ISGPF classification scheme. World J Surg. 2008;32(3):419-28.
Dirckx JH. Stedman's. Concise Medical Dictionary for The Health Professions Illustrated. Baltimore: Williams & Wilkins;1997.p.645.
Pedrazzoli S. Pancreatoduodenectomy (PD) and postoperative pancreatic fistula (POPF): A systematic review and analysis of the POPF-related mortality rate in 60,739 patients retrieved from the English literature published between 1990 and 2015. Medicine (Baltimore). 2017;96(19):367-42.
Karim SAM, Abdulla KS, Abdulkarim QH, Rahim FH. The outcomes and complications of pancreaticoduodenectomy (Whipple procedure): Cross sectional study. Int J Surg. 2018;52:383-7.
Bassi C, Dervenis C, Butturini G, Fingerhut A, Yeo C, Izbicki J, et al. Postoperative pancreatic fistula: an international study group (ISGPF) definition. Surgery. 2005;138(1):8-13.
Pratt WB, Maithel SK, Vanounou T, Huang ZS, Callery MP, Vollmer CM. Clinical and economic validation of the International Study Group of Pancreatic Fistula (ISGPF) classification scheme. Ann Surg. 2007;245(3):443-51.
McMillan MT, Vollmer CM, Asbun HJ, Ball CG, Bassi C, Beane JD, et al. The Characterization and Prediction of ISGPF Grade C Fistulas Following Pancreatoduodenectomy. J Gastrointest Surg. 2016;20(2):262-76.
Chen BP, Bennett S, Bertens KA, Balaa FK, Martel G. Use and acceptance of the International Study Group for Pancreatic Fistula (ISGPF) definition and criteria in the surgical literature. HPB (Oxford). 2018;20(1):69-75.
Nahm CB, Connor SJ, Samra JS, Mittal A. Postoperative pancreatic fistula: a review of traditional and emerging concepts. Clin Exp Gastroenterol. 2018;11:105-18.
Pulvirenti A, Ramera M, Bassi C. Modifications in the International Study Group for Pancreatic Surgery (ISGPS) definition of postoperative pancreatic fistula. Transl Gastroenterol Hepatol. 2017;2:107.
Bassi C, Buchler MW, Fingerhut A, Sarr M. Predictive factors for postoperative pancreatic fistula. Ann Surg. 2015;261(4):e99.
Mendoza AS, Han HS, Ahn S, Yoon YS, Cho JY, Choi Y. Predictive factors associated with postoperative pancreatic fistula after laparoscopic distal pancreatectomy: a 10-year single-institution experience. Surg Endosc. 2016;30(2):649-56.
Chen Y, Tian X, Xie X, Gao H, Zhuang Y, Yang Y. [Risk factors of postoperative pancreatic fistula after pancreaticoduodenectomy and its predictive score]. Zhonghua Wai Ke Za Zhi. 2016;54(1):39-43.
Napoli N, Kauffmann EF, Menonna F, Costa F, Iacopi S, Amorese G, et al. Robotic versus open pancreatoduodenectomy: a propensity score-matched analysis based on factors predictive of postoperative pancreatic fistula. Surg Endosc. 2018;32(3):1234-47.
Keck T, Wellner UF, Bahra M, Klein F, Sick O, Niedergethmann M, et al. Pancreatogastrostomy Versus Pancreatojejunostomy for Reconstruction After Pancreatoduodenectomy (RECOPANC, DRKS 00000767): Perioperative and Long-term Results of a Multicenter Randomized Controlled Trial. Ann Surg. 2016;263(3):440-9.
Malleo G, Pulvirenti A, Marchegiani G, Butturini G, Salvia R, Bassi C. Diagnosis and management of postoperative pancreatic fistula. Langenbecks Arch Surg. 2014;399(7):801-10.
Roberts KJ, Sutcliffe RP, Marudanayagam R, Hodson J, Isaac J, Muiesan P, et al. Scoring System to Predict Pancreatic Fistula After Pancreaticoduodenectomy: A UK Multicenter Study. Ann Surg. 2015;261(6):1191-7.
Qiu J, Du C. Pancreatogastrostomy versus Pancreatojejunostomy for Reconstruction After Pancreatoduodenectomy (RECOPANC, DRKS 00000767): Perioperative and Long-term Results of a Multicenter Randomized Controlled Trial. Ann Surg. 2017;266(6): 405-9.
Bassi C, Marchegiani G, Dervenis C, Sarr M, Abu Hilal M, Adham M, et al. The 2016 update of the International Study Group (ISGPS) definition and grading of postoperative pancreatic fistula: 11 Years After. Surgery. 2017;161(3):584-91.
Liu Y, Li Y, Wang L, Peng CJ. Predictive value of drain pancreatic amylase concentration for postoperative pancreatic fistula on postoperative day 1 after pancreatic resection: An updated meta-analysis. Medicine (Baltimore). 2018;97(38).
Crafa F, Esposito F, Noviello A, Moles N, Coppola Bottazzi E, Lombardi C, et al. How to prevent the postoperative pancreatic fistula with an ethylene vinyl alcohol copolymer (Onyx(R)): A proposal of a new technique. Ann Hepatobiliary Pancreat Surg. 2018;22(3):248-52.
Ke Z, Cui J, Hu N, Yang Z, Chen H, Hu J, et al. Risk factors for postoperative pancreatic fistula: Analysis of 170 consecutive cases of pancreaticoduodenectomy based on the updated ISGPS classification and grading system. Medicine (Baltimore). 2018;97(35):e12151.
Young S, Sung ML, Lee JA, DiFronzo LA, O'Connor VV. Pasireotide is not effective in reducing the development of postoperative pancreatic fistula. HPB (Oxford). 2018;20(9):834-40.
Chen CB, McCall NS, Pucci MJ, Leiby B, Dabbish N, Winter JM, et al. The Combination of Pancreas Texture and Postoperative Serum Amylase in Predicting Pancreatic Fistula Risk. Am Surg. 2018;84(6):889-96.
Hempel S, Puttmann P, Kahlert C, Seifert L, Mees ST, Welsch T, et al. [Outpatient Drain Management in Patients with Clinically Relevant Postoperative Pancreatic Fistula (CR-POPF) - Current Status in Germany]. Zentralbl Chir. 2018;143(3):270-7.
Yuksel A, Bostanci EB, Colakoglu MK, Ulas M, Ozer I, Karaman K, et al. Pancreatic stump closure using only stapler is associated with high postoperative fistula rate after minimal invasive surgery. Turk J Gastroenterol. 2018;29(2): 312-317.
Shi Y, Liu Y, Gao F, Liu Y, Tao S, Li Y, et al. Pancreatic Stiffness Quantified with MR Elastography: Relationship to Postoperative Pancreatic Fistula after Pancreaticoenteric Anastomosis. Radiology. 2018;288(2):476-84.
Nahm CB, Connor SJ, Samra JS, Mittal A. Postoperative pancreatic fistula: a review of traditional and emerging concepts. Clin Exp Gastroenterol. 2018;11:105-18.
Manipadam JM, Kadamapuzha JM. The Effect of Preoperative Biliary and Pancreatic Drainage on Postoperative Pancreatic Fistula: A Retrospective Cohort Study. Surg J (N Y). 2018;4(1):e37-e42.
Kantor O, Pitt HA, Talamonti MS, Roggin KK, Bentrem DJ, Prinz RA, et al. Minimally invasive pancreatoduodenectomy: ¿is the incidence of clinically relevant postoperative pancreatic fistula comparable to that after open pancreatoduodenectomy? Surgery. 2018;163(3):587-93.
Kamiya S, Hiki N, Kumagai K, Honda M, Nunobe S, Ohashi M, et al. Two-point measurement of amylase in drainage fluid predicts severe postoperative pancreatic fistula after gastric cancer surgery. Gastric Cancer. 2018;21(5):871-8.
Yang F, Jin C, Di Y, He H, Hao S, Yao L, et al. Central pancreatectomy with external drainage of monolayer pancreatojejunostomy for prevention of postoperative pancreatic fistula: A retrospective cohort study. Int J Surg. 2018;51:104-8.
Nahm CB, Brown KM, Townend PJ, Colvin E, Howell VM, Gill AJ, et al. Acinar cell density at the pancreatic resection margin is associated with post-pancreatectomy pancreatitis and the development of postoperative pancreatic fistula. HPB (Oxford). 2018;20(5):432-40.
Kawaida H, Kono H, Watanabe M, Hosomura N, Amemiya H, Fujii H. Risk factors of postoperative pancreatic fistula after distal pancreatectomy using a triple-row stapler. Surg Today. 2018;48(1):95-100.
Maggino L, Vollmer CM. Pasireotide for the Prevention of Postoperative Pancreatic Fistula: Time to Curb the Enthusiasm? Ann Surg. 2018;267(5):e94-e6.
Kuhara K, Shiozawa S, Usui T, Tsuchiya A, Miyauchi T, Kono T, et al. [Analysis of the Relationship between the Change of Drain Amylase Value and Postoperative Pancreatic Fistula after Pancreaticoduodenectomy]. Gan To Kagaku Ryoho. 2017;44(12):1729-31.
Wang H, Xiu D, Tao M. The pancreatic juice length in the stent tube as the predicting factor of clinical relevant postoperative pancreatic fistula after pancreaticoduodenectomy. Medicine (Baltimore). 2017;96(44):e8451.
Casadei R, Ricci C, Taffurelli G, Pacilio CA, Di Marco M, Pagano N, et al. Prospective validation of a preoperative risk score model based on pancreatic texture to predict postoperative pancreatic fistula after pancreaticoduodenectomy. Int J Surg. 2017;48:189-94.
Miyasaka Y, Mori Y, Nakata K, Ohtsuka T, Nakamura M. Attempts to prevent postoperative pancreatic fistula after distal pancreatectomy. Surg Today. 2017;47(4):416-24.
Bertens KA, Crown A, Clanton J, Alemi F, Alseidi AA, Biehl T, et al. What is a better predictor of clinically relevant postoperative pancreatic fistula (CR-POPF) following pancreaticoduodenectomy (PD): postoperative day one drain amylase (POD1DA) or the fistula risk score (FRS)? HPB (Oxford). 2017;19(1):75-81.
Williamsson C, Ansari D, Andersson R, Tingstedt B. Postoperative pancreatic fistula-impact on outcome, hospital cost and effects of centralization. HPB (Oxford). 2017;19(5):436-42.
Jover JM, Carabias A, Fuerte S, Ríos R, Ortega I, Limones M. Resultados de la derivación con 2 asas tras duodenopancreatectomía cefálica. Cir Esp. 2006;80(6):373-7.
Enlaces refback
- No hay ningún enlace refback.

Esta obra está bajo una licencia de Creative Commons Reconocimiento-NoComercial-CompartirIgual 4.0 Internacional.










 La Revista está: Certificada por el CITMA
La Revista está: Certificada por el CITMA Acreditados como: "Web de Interés Sanitario"
Acreditados como: "Web de Interés Sanitario"
