Non-pharmacological techniques in the management of behavior before the dental treatment of the child
Abstract
Introduction: Many times the experience of the child finds a way to respond to a problem in a more credible way, being more real than the attention of the child's clinic is combined.
Objective: To determine the effectiveness of these techniques in the control of anxiety in children before dental treatment.
Methods: It was an experimental and quantitative subject; a sample population of 16 children from 6 to 11 years of age was taken. Which were made for intervention with non-pharmacological techniques.
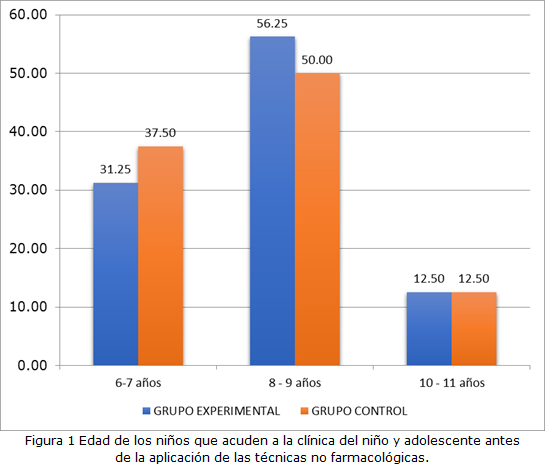
Results: After the analysis, the t-Student test was used, which is 56.25 % of the children of the experimental group and 50 % of the control group are in the age range of 8 to 9 years, 31.25% and 37.5% between 6 to 7 years and 12.50 % in both groups from 10 to 11 years respectively; unlike the control group, 75 % of the children before the care presented high anxiety, after which 68.75 % presented moderate anxiety.
Conclusions: Non-pharmacological techniques are effective in managing behaviors in the dental office, unlike children in the control group without this intervention, they decrease to a moderate level.
DeCS: CHILD; DENTAL ANXIETY; ANXIETY; COMPLEMENTARY THERAPIES; TREATMENT OUTCOME.
Downloads
References
1. Leko J, ? krinjarić T, Goršeta K. Reliability and Validity of Scales for Assessing Child Dental Fear and Anxiety. Acta Stomatol Croat [Internet]. 2020 [citado 29 Ene 2022];54(1):22-31. Disponible en: https://ascro.hr/wp-content/uploads/2020/04/3-Leko-2020-1.pdf
2. Padding AM, Rutjes NW, Hashimoto S, Vos A, Staphorst MS, van Aalderen WMC, et al. Young children experience little emotional burden during invasive procedures in asthma research. Eur J Pediatr [Internet]. 2019 [citado 29 Ene 2022];178(2):207-211. Disponible en: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6339656/
3. Wu L, Buchanan H, van Wijk AJ. Translation and Validation of the Short Form of the Fear of Dental Pain Questionnaire in China. Front Psychol [Internet]. 2021 Nov [citado 29 Ene 2022];12:721670. Disponible en: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC8649632/
4. Cianetti S, Lombardo G, Lupatelli E, Pagano S, Abraha I, Montedori A, et al. Dental fear/anxiety among children and adolescents. A systematic review. Eur J Paediatr Dent. 2017 Jun;18(2):121-130. doi:10.23804/ejpd.2017.18.02.07.
5. Martignon S, Cortes A, Douglas GVA, Newton JT, Pitts NB, Avila V, et al. Caries Care International adapted for the pandemic in children: Caries OUT multicentre single-group interventional study protocol. BMC Oral Health [Internet]. 2021 Jul [citado 29 Sep 2022];21(1):329. Disponible en: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC8248759/
6. Kumar A, Zubair M, Gulraiz A, Kalla S, Khan S, Patel S, et al. An Assessment of Risk Factors of Delayed Speech and Language in Children: A Cross-Sectional Study. Cureus [Internet]. 2022 Sep [citado 29 Sep 2022];14(9):e29623. Disponible en: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC9608900/
7. Munayco Pantoja ER, Mattos-Vela MA, Torres Ramos G, Blanco Victorio DJ. Relación entre ansiedad, miedo dental de los padres y la colaboración de niños al tratamiento odontológico. ODOVTOS-Int J Dental Sc [Internet]. 2018 [citado 29 Ene 2022];1(20-3):81-91. Disponible en: https://www.scielo.sa.cr/pdf/odovtos/v20n3/2215-3411-odovtos-20-03-81.pdf
8. Bajrić E, Kobašlija S, Huseinbegović A, Zukanović A, Marković N, Selimović-Dragaš M, et al. Predictors of Dental Fear and Anxiety in 9-12-year-old Children in Bosnia and Herzegovina. Acta Stomatol Croat [Internet]. 2022 Sep [citado 29 Ene 2022];56(3):246-56. Disponible en: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC9635503/
9. Nazari N, Shabbir MS, Sevbitov AV, Sadeghi M, Griffiths MD. Psychometric evaluation of the Russian version of the Gaming Disorder Scale for Adolescents. Current Psychology [Internet]. 2022 [citado 29 Ene 2022];42(2023):13754-68. Disponible en: https://link.springer.com/article/10.1007/s12144-021-02575-w
10. Abanto Alvarez J, Pinto e Carvalho Rezende KM, Bönecker M, Nahas Pires Corrêa F, Salete Nahás Pires Correa M. Propuestas no-farmacológicas de manejo del comportamiento en niños. Rev Estomatol Herediana [Internet]. 2010 Abr-Jun [citado 29 Sep 2022];20(2):101-6. Disponible en: https://www.redalyc.org/pdf/4215/421539358009.pdf
11. Benito A, Calvo G, Real-López M, Gallego MJ, Francés S, Turbi Á, et al. Creation of the TXP parenting questionnaire and study of its psychometric properties. Adicciones. 2019 Abr;31(2):117-35. doi:10.20882/adicciones.983
12. Wright N, Pickles A, Sharp H, Hill J. A psychometric and validity study of callous-unemotional traits in 2.5-year-old children. Sci Rep [Internet]. 2021 [citado 29 Sep 2022];11(2021):8065. Disponible en: https://www.nature.com/articles/s41598-021-87416-3
13. Cuthberg MI, Melamend BG. A screening device: children at risk for dental fears and management problems. J Dent Child [Internet]. 1982 Nov-Dic [citado 29 Ene 2022];49(6):432-6. Disponible en: https://pubmed.ncbi.nlm.nih.gov/6960031/
14. Buchanan H. Development of a computerised dental anxiety scale for children: validation and reliability. Br Dent J [Internet]. 2005 Sep [citado 29 Sep 2022];199(6):359-62. Disponible en: https://www.nature.com/articles/4812694
15. Organización Panamericana de la Salud. Programa de Educación Continuada Odontológica No Convencional [Internet]. Washington, DC: OPS; 1999 [citado 29 Sep 2022]. Disponible en: https://iris.paho.org/bitstream/handle/10665.2/3117/Curso%2520I%2520Odontologia%2520preventiva.%2520Modulo%25203%2520Medidas%2520y%2520programas%2520preventivos.pdf?sequence=1&isAllowed=y
16. Babaji P, Chauhan P, Churasia VR, Kaur T, Singh S, Augustine M. A cross-sectional evaluation of children preference for dentist attire and syringe type in reduction of dental anxiety. Dent Res J [Internet]. 2018 Nov-Dic [citado 29 Ene 2022];15(6):391-6. Disponible en: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6243804/
17. Garrocho-Rangel JA, Ruiz-Rodríguez MS, Pozos-Guillén AJ. Fundamentals in Biostatistics for Research in Pediatric Dentistry: Part I - Basic Concepts. J Clin Pediatr Dent [Internet]. 2017 [citado 29 Sep 2022];41(2):87-94. Disponible en: https://oss.jocpd.com/files/article/20220708-341/pdf/JOCPD41.2.87.pdf
18. Garrocho-Rangel A, Ruiz-Rodríguez S, Gaitán-Fonseca C, Pozos-Guillén A. Randomized Clinical Trials in Pediatric Dentistry: Application of Evidence-Based Dentistry through the CONSORT Statement. J Clin Pediatr Dent [Internet]. 2019 [citado 29 Sep 2022];43(4):219-30. Disponible en: https://oss.jocpd.com/files/article/20220630-160/pdf/1053-4625-43_4_1.pdf
19. Marcano AA, Figueredo AM, Orozco G. Evaluación de la ansiedad y miedo en niños escolares en la consulta odontopediátrica. Rev Odontopediatria Latinoam [Internet]. 2012 Jul-Dic [citado 29 Sep 2022];2(2):1-10. Disponible en: https://www.revistaodontopediatria.org/index.php/alop/article/view/65/173
20. Jiang YN, Wang JX, Chen LY, Yao JJ, Ni L, Sheng JM. Reliability and Validity of the Composite Activity-Related Fall Risk Scale. Front Neurol [Internet]. 2022 Mar [citado 29 Ene 2022];13:832691. Disponible en: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC8980318/
21. Quek JS, Lai B, Yap AU, Hu S. Non-pharmacological management of dental fear and anxiety in children and adolescents: An umbrella review. Eur J Paediatr Dent. 2022 Sep;23(3):230-42. doi:10.23804/ejpd.2022.23.03.11.
22. Carrillo-Díaz M, Migueláñez-Medrán BC, Nieto-Moraleda C, Romero-Maroto M, González-Olmo MJ. How Can We Reduce Dental Fear in Children? The Importance of the First Dental Visit. Children [Internet]. 2021 Dic [citado 29 Sep 2022];8(12):1167. Disponible en: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC8700154/
23. Kroniņa L, Rasčevska M, Care R. Psychosocial factors correlated with children's dental anxiety. Stomatologija [Internet]. 2017 [citado 29 Ene 2022];19(3):84-90. Disponible en: https://sbdmj.lsmuni.lt/173/173-03.pdf
24. Pop-Jordanova N. Different Clinical Expression of Anxiety Disorders in Children and Adolescents: Assessment and Treatment. Pril (Makedon Akad Nauk Umet Odd Med Nauki) [Internet]. 2019 May [citado 29 Ene 2022];40(1):5-40. Disponible en: https://sciendo.com/article/10.2478/prilozi-2019-0001
25. Lin M, Thornton-Evans G, Griffin SO, Wei L, Junger M, Espinoza L. Increased Dental Use May Affect Changes in Treated and Untreated Dental Caries in Young Children. JDR Clin Trans Res [Internet]. 2019 Ene [citado 29 Sep 2022];4(1):49-57. Disponible en: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC8928738/
26. Cebalo N, Negovetić Vranić D, Bašić Kes V. The Effect of Transcutaneous Electric Nerve Stimulation (TENS) on Anxiety and Fear in Children Aged 9-14 Years. Acta Stomatol Croat [Internet]. 2020 Dic [citado 29 Sep 2022];54(4):412-9. Disponible en: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7871430/
27. Szeska C, Richter J, Wendt J, Weymar M, Hamm AO. Promoting long-term inhibition of human fear responses by non-invasive transcutaneous vagus nerve stimulation during extinction training. Sci Rep [Internet]. 2020 [citado 29 Sep 2022];10:1529. Disponible en: https://www.nature.com/articles/s41598-020-58412-w
28. Kheir OO, Ziada HM, Abubakr NH, Abdel-Rahman ME, Fadl SM, Ibrahim YE. Patient-dentist relationship and dental anxiety among young Sudanese adult patients. Int Dent J [Internet]. 2019 Feb [citado 29 Sep 2022];69(1):35-43. Disponible en: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC9378979/
29. Sivaramakrishnan G, Makki H, AlDallal S, Alaswad Z, Sultan E, Ahmed S, et al. The variables associated with dental anxiety and their management in primary care dental clinics in Bahrain: a cross-sectional study. BMC Oral Health [Internet]. 2022 Abr [citado 29 Sep 2022];22(1):137. Disponible en: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC9026669/
Published
How to Cite
Issue
Section
License
Copyright (c) 2023 Ronald Rosendo Enriquez-Quispe, Britto Ebert Falcón-Guerrero, Henry Quispe-Cruz

This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License.
Copyright: Camagüey Medical Archive Magazine, offers immediately after being indexed in the SciELO Project; Open access to the full text of the articles under the principle of making available and free the research to promote the exchange of global knowledge and contribute to a greater extension, publication, evaluation and extensive use of the articles that can be used without purpose As long as reference is made to the primary source.
Conflicts of interest: authors must declare in a mandatory manner the presence or not of conflicts of interest in relation to the investigation presented.
(Download Statement of potential conflicts of interest)
The Revista Archivo Médico de Camagüey is under a License Creative Commons Attribution-Noncommercial-No Derivative Works 4.0 International (CC BY 4.0).
This license allows others to distribute, to mix, to adjust and to build from its work, even for commercial purposes, as long as it is recognized the authorship of the original creation. This is the most helpful license offered. Recommended for maximum dissemination and use of licensed materials. The full license can be found at: https://creativecommons.org/licenses/












 22 julio 2025
22 julio 2025