Principles of Kirschner fixation in supracondylar humeral fractures in children
Abstract
Introduction: Supracondylar humeral fractures in children are frequent injuries. The treatment of these injuries is generally a surgical one through closed or open reduction and placement of Kirschner wires.
Objective: To update and provide information on Kirschner wire fixation in pediatric patients with supracondylar humeral fractures.
Methods: The search and analysis of the information was carried out in a period of 61 days (September 1st to October 31st, 2022) and the following words were used: pediatric supracondylar humeral fractures AND pinning, pinning configuration, pinning loosening AND pediatric supracondylar fractures. To focus the search, the Boolean OR or AND operators were used as appropriate. Based on the information obtained, a bibliographic review of a total of 211 articles published in the PubMed, Hinari, SciELO and Medline databases was carried out using the search reference manager EndNote. Of which 38 selected citations were used to conduct the review, all from the last five years.
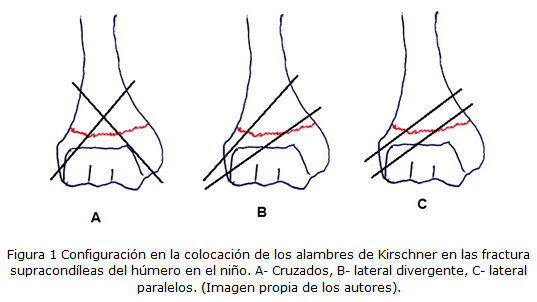
Results: References are made to the types of Kirschner wire used for this kind of fracture fixation. The most widely used wire configurations are mentioned, such as two lateral wires followed by crossed fixation. The most frequent errors in the placement of the wires are exposed, in addition to the complications related to this surgical procedure.
Conclusions: In general, supracondylar humeral fractures in children require surgical management. The closed reduction through the placement of percutaneous Kirschner wires, require specific technical knowledge.
DeCS: HUMERAL FRACTURES, DISTAL/SURGERY; HUMERAL FRACTURES, DISTAL/ COMPLICATIONS; CHILD; BONE WIRES; MEDICAL ERRORS.
Downloads
References
1. Chong HH, Qureshi A. Pediatric distal humeral supracondylar fracture - achievement of optimal pinning configuration. Acta Orthop Belg [Internet]. 2022 Jun [citado 26 Sep 2022];88(2):245-54. Disponible en: https://pubmed.ncbi.nlm.nih.gov/36001829/
2. Hosseinzadeh P, Rickert KD, Edmonds EW. What's new in pediatric orthopaedic trauma: the upper extremity. J Pediatr Orthop [Internet]. 2020 Apr [citado 26 Sep 2022];40(4): [aprox.3 p.]. Disponible en: https://pubmed.ncbi.nlm.nih.gov/31145183/
3. Silverstein RS, Meltsakos CP, Dedhia N, Lynch BC, Lucas PA, Asprinio DE, et al. Range of motion following percutaneous fixation of pediatric supracondylar humerus fracture is independent of anterior osseous fragment resorption. J Pediatr Orthop B [Internet]. 2022 Jan [citado 26 Sep 2022];31(1):[aprox.6 p.]. Disponible en: https://pubmed.ncbi.nlm.nih.gov/33315806/
4. Abousaleh MA, Zeidan AA, Mukhtar I, Keshta AS, Aladraj TH, Shaaban OA, et al. Comparative effectiveness of closed reduction with percutaneous pinning and open reduction with internal fixation in the operative management of pediatric type III supracondylar fractures. Cureus [Internet]. 2022 Feb [citado 26 Sep 2022];14(2):e22707. Disponible en: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC8967402/
5. Zhao H, Xu S, Liu G, Zhao J, Wu S, Peng L. Comparison of lateral entry and crossed entry pinning for pediatric supracondylar humeral fractures: a meta-analysis of randomized controlled trials. J Orthop Surg Res [Internet]. 2021 Jun [citado 26 Sep 2022];16: 366. Disponible en: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC8188794/
6. Poggiali P, Nogueira FCS, Nogueira MPM. Management of Supracondylar Humeral Fracture in Children. Rev Bras Ortop [Internet]. 2022 Feb [citado 26 Sep 2022]; 57(1): 23-32. Disponible en: https://www.thieme-connect.com/products/ejournals/abstract/
10.1055/s-0040-1709734
7. Eguia F, Gottlich C, Lobaton G, Vora M, Sponseller PD, Lee RJ. Mid-term Patient-reported Outcomes After Lateral Versus Crossed Pinning of Pediatric Supracondylar Humerus Fractures. J Pediatr Orthop [Internet]. 2020 Ago [citado 26 Sep 2022];40(7):323-8. Disponible en: https://pubmed.ncbi.nlm.nih.gov/32271317/
8. Kwok SM, Clayworth C, Nara N. Lateral versus cross pinning in paediatric supracondylar humerus fractures: a meta-analysis of randomized control trials. ANZ J Surg [Internet]. 2021 May [citado 26 Sep 2022];91(5):980-5. Disponible en: https://pubmed.ncbi.nlm.nih.gov/33792121/
9. Heffernan MJ, Lucak T, Igbokwe L, Yan J, Gargiulo D, Khadim M. The Reverse Oblique Supracondylar Humerus Fracture: Description of a Novel Fracture Pattern. J Pediatr Orthop [Internet]. 2020 Feb [citado 26 Sep 2022];40(2):e131-e137. Disponible en: https://pubmed.ncbi.nlm.nih.gov/31022014/
10. Shah M, Han JH, Park H, Kim HW, Park KB. Prevalence and Treatment Outcome of Displaced High-Long Oblique Supracondylar Humeral Fractures in Children. Front Pediatr [Internet]. 2021 [citado 26 Sep 2022];9:739909. Disponible en: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC8578841/
11. Catena N, Calevo MG, Fracassetti D, Moharamzadeh D, Origo C, De Pellegrin M. Risk of ulnar nerve injury during cross-pinning in supine and prone position for supracondylar humeral fractures in children: a recent literature review. Eur J Orthop Surg Traumatol [Internet]. 2019 Ago [citado 26 Sep 2022];29(6):[aprox.6 p.]. Disponible en: https://link.springer.com/article/10.1007/s00590-019-02444-0
12. Venkatadass K, Maji M, Sangeet G, Raghavendra K, Rajasekaran S. Factors determining loss of reduction in paediatric supracondylar humerus fractures treated by closed reduction and percutaneous pinning. J Pediatr Orthop B [Internet]. 2022 May [citado 26 Sep 2022];31(3):289-95. Disponible en: https://pubmed.ncbi.nlm.nih.gov/34285159/
13. Linsay SE, Holmes S, Owen J, Swarup I, Halsey M. The Pin: An Orthopaedic Transformation. JPOSNA [Internet]. 2022 May [citado 26 Sep 2022];4(2). Disponible en: https://www.jposna.org/~jposna/index.php/jposna/article/view/448/656
14. Bekmez S, Camp MW, Ling R, El-Amiri N, Howard AW. Supracondylar Humerus Fractures in older Children: Success of Closed Reduction and Percutaneous Pinning. J Pediatr Orthop [Internet]. 2021 Abr [citado 26 Sep 2022];41(4):242-48. Disponible en: https://pubmed.ncbi.nlm.nih.gov/33655902/
15. Wei YS, Liu WL, Bai R, Li DH, Zhao ZQ, Wang Y, et al. The use of a transolecranon pin joystick technique in the treatment of multidirectionally unstable supracondylar humeral fractures in children. J Pediatr Orthop B. 2020;29(5):452-7. doi: 10.1097/BPB.0000000000000787.
16. Wendling-Keim DS, Binder M, Dietz HG, Lehner M. Prognostic Factors for the Outcome of Supracondylar Humeral Fractures in Children. Orthop Surg [Internet]. 2019 Ago [citado 26 Sep 2022];11(4):690-7. Disponible en: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6712406/
17. Claireaux H, Goodall R, Hill J, Wilson E, Coull P, Green S, et al. Multicentre collaborative cohort study of the use of Kirschner wires for the management of supracondylar fractures in children. Chin J Traumatol [Internet]. 2019 Oct [citado 26 Sep 2022];22(5):249-54. Disponible en: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6823708/
18. Radaideh AM, Rusan M, Obeidat O, Al-Nusair J, Albustami IS, Mohaidat ZM, et al. Functional and radiological outcomes of different pin configuration for displaced pediatric supracondylar humeral fracture: A retrospective cohort study. World J Orthop [Internet]. 2022 Mar [citado 26 Sep 2022];13(3):250-8. Disponible en: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC8935329/
19. Wang W, Li Q, Kamara A, Han Z, Liu T, Wang E. Analysis of the location and trajectory of the Kirschner wires in the fixation of extension-type supracondylar fracture of the humerus by 3D computational simulation. J Shoulder Elbow Surg [Internet]. 2022 Jul [citado 26 Sep 2022];31(7):1368-75. Disponible en: https://pubmed.ncbi.nlm.nih.gov/35151881/
20. Hannonen J, Pokka T, Serlo W, Sinikumpu JJ. Lateral-Only Kirschner-Wire Fixation of type-3 Supracondylar Humerus Fractures in Children with a Special Attention to Technical Issues. Scand J Surg [Internet]. 2021 Jun [citado 26 Sep 2022];110(2):258-64. Disponible en: https://pubmed.ncbi.nlm.nih.gov/32116116/
21. Na Y, Bai R, Zhao Z, Han C, Kong L, Ren Y, et al. Comparison of lateral entry with crossed entry pinning for pediatric supracondylar humeral fractures: a meta-analysis. J Orthop Surg Res [Internet]. 2018 [citado 26 Sep 2022];13:68. Disponible en: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5883290/
22. Rehm A, Ashby E, Granger L, Ong JCY. Comparison of lateral entry and crossed entry pinning for pediatric supracondylar humerus fractures: a meta-analysis of randomized controlled trials. J Orthop Surg Res [Internet]. 2022 Ago [citado 26 Sep 2022];17(1):[aprox.4 p.]. Disponible en: https://josr-online.biomedcentral.com/articles/
10.1186/s13018-022-03286-z
23. Uzer G, Yildiz F, Elmadag M, Bilsel K, Erden T, Pulatkan A, et al. Comparison of the lateral and posterior approaches in the treatment of pediatric supracondylar humeral fractures. J Pediatr Orthop B [Internet]. 2018 Mar [citado 26 Sep 2022];27(2):108-114. Disponible en: https://pubmed.ncbi.nlm.nih.gov/28328740/
24. Dineen HA, Stone J, Ostrum RF. Closed Reduction Percutaneous Pinning of a Pediatric Supracondylar Distal Humerus Fracture. J Orthop Trauma [Internet]. 2019 Ago [citado 26 Sep 2022];33(Suppl 1):S7-S8. Disponible en: https://journals.lww.com/jorthotrauma/Fulltext/2019/08001/Closed_Reduction_Percutaneous_Pinning_of_a.5.aspx
25. Bitzer AM, Belkoff SM, LiBrizzi CL, Chibututu C, Lee RJ. Sagittal plane alignment affects the strength of pin fixation in supracondylar humerus fractures. Medicine (Baltimore) [Internet]. 2021 Jun [citado 26 Sep 2022];100(22):e26173. Disponible en: https://pubmed.ncbi.nlm.nih.gov/34087880/
26. Rees AB, Schultz JD, Wollenman LC, Moore-Lotridge SN, Martus JE, Schoenecker JG, et al. A Mini-Open Approach to Medial Pinning in Pediatric Supracondylar Humeral Fractures May Be Safer Than Previously Thought. J Bone Joint Surg Am [Internet]. 2022 Ene [citado 26 Sep 2022];104(1):33-40. Disponible en: https://pubmed.ncbi.nlm.nih.gov/34673662/
27. Rupp M, Schäfer C, Heiss C, Alt V. Pinning of supracondylar fractures in Children - Strategies to avoid complications. Injury [Internet]. 2019 Jun [citado 26 Sep 2022];50 (Suppl 1):S2-S9. Disponible en: https://www.sciencedirect.com/science/article/abs/pii/S0020138319301603?via%3Dihub
28. Wong KPL, Chew EM, Mahadev A. Sliding the Medial Pin: A Safer Approach to Cross-pinning Humerus Supracondylar Fractures? Tech Hand Up Extrem Surg [Internet]. 2019 Sep [citado 26 Sep 2022];23(3):111-4. Disponible en: https://pubmed.ncbi.nlm.nih.gov/30664066/
29. Prusick VW, Gibian JT, Ross KE, Moore-Lotridge SN, Rees AB, Mencio GA, et al. Surgical Technique: Closed Reduction and Percutaneous Pinning of Posterolaterally Displaced Supracondylar Humerus Fractures. J Orthop Trauma [Internet]. 2021 Mar [citado 26 Sep 2022];35(3):e108-e115. Disponible en: https://pubmed.ncbi.nlm.nih.gov/32569073/
30. Tarallo L, Novi M, Porcellini G, Schenetti C, Micheloni GM, Maniscalco P, et al. Gartland type III supracondylar fracture in children: is open reduction really a dangerous choice? Injury [Internet]. 2022 Mar [citado 26 Sep 2022]; 53(Suppl 1): S13-S18. Disponible en: https://pubmed.ncbi.nlm.nih.gov/33678463/
31. Hendrych J, HavrÁnek P, CepelÍk M, Pe? l T. Advantages and Pitfalls of Stabilisation of Supracondylar Humerus Fractures in Children by Lateral Approach Only. Acta Chir Orthop Traumatol Cech [Internet]. 2020 [citado 26 Sep 2022];87(6):414-420. Disponible en: https://pubmed.ncbi.nlm.nih.gov/33408007/
32. Mitchell SL, Sullivan BT, Ho CA, Abzug JM, Raad M, Sponseller PD. Pediatric Gartland Type-IV Supracondylar Humeral Fractures Have Substantial Overlap with Flexion-Type Fractures. J Bone Joint Surg Am [Internet]. 2019 Ago [citado 26 Sep 2022];101(15):1351-6. Disponible en: https://pubmed.ncbi.nlm.nih.gov/31393425/
33. Jenkins SM, Mehlman CT, Denning JR. Unicolumnar Pin Fixation of Type III Supracondylar Humeral Fractures Is Associated With Over 3 Times Higher Odds of Lost Reduction. J Orthop Trauma [Internet]. 2022 Ene [citado 26 Sep 2022];36(1):e30-e34. Disponible en: https://pubmed.ncbi.nlm.nih.gov/34001803/
34. Rees AB, Schultz JD, Wollenman LC, Moore-Lotridge SN, Martus JE, Mencio GA, et al. Internal Rotation Stress Test Reduces Cross-Pinning and Improves Outcomes in Displaced Pediatric Supracondylar Humeral Fractures. JB JS Open Access [Internet]. 2021 Jul [citado 26 Sep 2022]; 6(3): [aprox.4 p.]. Disponible en: https://pubmed.ncbi.nlm.nih.gov/34337285/
35. Tokyay A, Okay E, Cansü E, Aydemir AN, Erol B. Effect of fracture location on rate of conversion to open reduction and clinical outcomes in pediatric Gartland type III supracondylar humerus fractures. Ulus Travma Acil Cerrahi Derg [Internet]. 2022 Jan [citado 26 Sep 2022];28(2):[aprox.6 p.]. Disponible en: https://tjtes.org/jvi.aspx?pdir=travma&plng=eng&un=UTD-23358
36. Vuillermin C, May C, Kasser J. Closed reduction and percutaneous pinning of pediatric supracondylar humeral fractures. JBJS Essent Surg Tech [Internet]. 2018 Apr [citado 26 Sep 2022];8(2):[aprox.4 p.]. Disponible en: https://pubmed.ncbi.nlm.nih.gov/30233982/
37. Sanders J, Goldstein RY. Open Reduction and Pin Fixation of Pediatric Lateral Humeral Condylar Fractures. JBJS Essent Surg Tech [Internet]. 2020 Nov [citado 26 Sep 2022]; 10(4): e19.00066. Disponible en: https://pubmed.ncbi.nlm.nih.gov/34055470/
38. Uludag A, Tosun HB, Aslan TT, Uludag Ö, Gunay A. Comparison of Three Different Approaches in Pediatric Gartland Type 3 Supracondylar Humerus Fractures Treated With Cross-Pinning. Cureus [Internet]. 2020 Jun [citado 26 Sep 2022];12(6):e8780. Disponible en: https://pubmed.ncbi.nlm.nih.gov/32596093/
Published
How to Cite
Issue
Section
License
Copyright (c) 2022 Alejandro Alvarez-López, Valentina Valdebenito-Aceitón, Sergio Ricardo Soto-Carrasco

This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License.
Copyright: Camagüey Medical Archive Magazine, offers immediately after being indexed in the SciELO Project; Open access to the full text of the articles under the principle of making available and free the research to promote the exchange of global knowledge and contribute to a greater extension, publication, evaluation and extensive use of the articles that can be used without purpose As long as reference is made to the primary source.
Conflicts of interest: authors must declare in a mandatory manner the presence or not of conflicts of interest in relation to the investigation presented.
(Download Statement of potential conflicts of interest)
The Revista Archivo Médico de Camagüey is under a License Creative Commons Attribution-Noncommercial-No Derivative Works 4.0 International (CC BY 4.0).
This license allows others to distribute, to mix, to adjust and to build from its work, even for commercial purposes, as long as it is recognized the authorship of the original creation. This is the most helpful license offered. Recommended for maximum dissemination and use of licensed materials. The full license can be found at: https://creativecommons.org/licenses/












 22 julio 2025
22 julio 2025