Epidemiological, clinical and laboratory characterization in persistent positive COVID-19 patients
Abstract
Introduction: COVID-19 is a global concern, it requires a comprehensive approach to reduce transmission, starting with case detection, hospital care and subsequent follow-up.
Objective: To characterize persistent COVID-19 positive patients in terms of epidemiology, clinical and laboratory data.
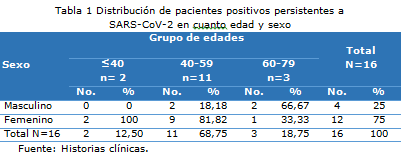
Methods: A cross-sectional descriptive study was carried out in 16 persistent SARS-CoV-2 positive patients diagnosed by RT-CPR in nasopharyngeal swab, at Comandante Manuel Fajardo Rivero Hospital of Santa Clara in the period from September 2020 to November 2020.
Results: The female sex predominated in 75%, the most representative age group was 40-59 years of age (68.75%), 37.50% of the cases were asymptomatic and the most frequent symptom was fever less than seven days 31.25%. There was lymphopenia in the initial hemogram with an average of 27.49, and a leukocyte neutrophil index above three in 4 patients with an initial average of 3.42. Hospital stay of 20.75 days on average. Half had no history of known disease, the most frequent comorbidity was arterial hypertension 43.75 %. The neutrophil leukocyte index above 3 in patients with comorbidities, evolutionary for all pariente was less than 3.
Conclusions: The female sex predominates, the most representative age group is 40-59 years, it is frequent that they present asymptomatic and fever is the most usual symptom. There is lymphopenia on the initial blood count. Half of those infected without comorbidities. The evolutionary leukocyte neutrophil index was less than 3 for all patients.
DeCS: COVID-19/epidemiology; SARS-CoV-2; COMORBIDITY; REVERSE TRANSCRIPTASE POLYMERASE CHAIN REACTION; SECONDARY CARE.
Downloads
References
1. Pan L, Wang R, Yu N, Hu C, Yan J, Zang X, et al. Clinical characteristics of re-hospitalized COVID-19 patients with recurrent positive SARS-CoV-2 RNA: a retrospective study. Eur J Clin Microbiol Infect Dis [Internet]. 2021 [citado 06 Sep 2021];40(6):1245-52. Disponible en: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7808928/
2. Jianghong A, Xuejiao L, Tongyang X, Shen Q, Jing Y, Haocheng Y et al. Clinical characteristics of recovered COVID-19 patients with re-detectable positive RNA test. Ann Transl Med [Internet]. 2020 [citado 06 Sept 2021];8(17):1084-9. Disponible en: https://pubmed.ncbi.nlm.nih.gov/33145303/
3. Wan R, Mao ZQ, He LY, Hu YC, Chen W. Evidence from two cases of asymptomatic infection with SARS-CoV-2: Are 14 days of isolation sufficient?. Int J Infect Dis [Internet]. 2020 Jun [citado 06 Sep 2021];95:174-5. Disponible en: https://www.sciencedirect.com/science/article/pii/S1201971220301739
4. Ulhaq ZS, Soraya GV, Fauziah FA. Test ARN para SARS-CoV-2 positivos recurrentes en pacientes recuperados y dados de alta hospitalaria. Rev Clin Esp [Internet]. 2020 Nov [citado 06 Sep 2021];220(8):524-6. Disponible en: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7342044/
5. Basbus L, Lapidus MI, Martingano I, Puga MC, Pollán J. Índice neutrófilo-linfocito como factor pronóstico de COVID-19. MEDICINA [Internet]. 2020 [citado 06 sept 2021];80(Suppl 3):31-6. Disponible en: https://www.medicinabuenosaires.com/revistas/vol80-20/s3/31.pdf
6. Díaz-Rodríguez YL, Quintana-López LA. SARS-CoV-2, ¿reinfección o diseminación viral persistente? Rev cuban invest bioméd [Internet]. 2021 [citado 06 Sep 2021];40(1). Disponible en: https://revibiomedica.sld.cu/index.php/ibi/article/view/1156/947
7. Saurabh S, Kumar R, Gupta MK, Bhardwaj P, Nag VL, Garg MK, et al. Prolonged persistence of SARS-CoV-2 in the upper respiratory tract of asymptomatic infected individuals. QJM [Internet]. 2020 Ago [citado 06 Sep 2021];113(8):556–60. Disponible en: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7337859/
8. Li J, Wei X, Tian W, Zou J, Wang Y, Xue W, et al. Clinical features of discharged COVID-19 patients with an extended SARSCoV-2 RNA positive signal in respiratory samples. Virus Res [Internet]. 2020 Sep [citado 06 Sep 2021];286:198047. Disponible en: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7833058/
9. Cento V, Colagrossi L, Nava A, Lamberti A, Senatore S, Travi G, et al. Persistent positivity and fluctuations of SARS-CoV-2 RNA in clinically recovered COVID-19 patients. J Infect [Internet]. 2020 Sep [citado 06 Sep 2021];81(3):e90-e92. Disponible en: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7836522/
10. Lan L, Xu D, Ye G, Xia G, Wang S, Li Y, et al. Positive RT-PCR Test Results in Patients Recovered From COVID-19. JAMA [Internet]. 2020 Abr [citado 06 Sep 2021];323(15):1502-3. Disponible en: https://pubmed.ncbi.nlm.nih.gov/32105304/
11. Gombar S, Chang M, Hogan CA, Zehnder J, Boyd S, Pinsky BA, et al. Persistent detection of SARS-CoV-2 RNA in patients and healthcare workers with COVID-19. J Clin Virol [Internet]. 2020 Ago [citado 06 Sep 2021];129:104477. Disponible en: https://pubmed.ncbi.nlm.nih.gov/32505778/
12. Peng J, Wang M, Zhang M, Lu E. Seven discharged patients turning positive again for SARS-CoV-2 on quantitative RT-PCR. Am J Infect Control [Internet]. 2020 Jun [citado 06 Sep 2021];48(6):725-6. Disponible en: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7151314/
13. Yahav D, Yelin D, Eckerle I, Eberhardt C, Wang J, Cao B, et al. Definitions for coronavirus disease 2019 reinfection, relapse and PCR re-positivity. Clin Microbiol Infect [Internet]. 2021 Mar [citado 06 Sep 2021];27(3):315-8. Disponible en: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7718119/
14. Ikegami S, Benirschke R, Flanagan T, Tanna N, Klein T, Elue R, et al. Persistence of SARS-CoV-2 nasopharyngeal swab PCR positivity in COVID-19 convalescent plasma donors. Transfusion [Internet]. 2020 Dic [citado 06 Sep 2021];60(12):2962-8. Disponible en: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7461313/
15. Osman S, Al Daajani MM, Alsahafi AJ. Re-positive coronavirus disease 2019 PCR test: could it be a reinfection? New Microbes New Infect [Internet]. 2020 Sep [citado 06 Sep 2021];37:100748. Disponible en: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7439804/
16. Barrios Osuna I, Anido Escobar V, Morera Pérez M. Declaración de Helsinki: cambios y exégesis. Rev cuba salud pública [Internet]. 2016 [citado 06 Sep 2021];42(1). Disponible en: https://revsaludpublica.sld.cu/index.php/spu/article/view/597/491
17. Guan W, Ni Z, Hu Y, Liang W, Ou C, He J, et al. Clinical Characteristics of Coronavirus Disease 2019 in China. J Emerg Med [Internet]. 2020 Abr [citado 06 Sep 2021];58(4):711-2. Disponible en: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7266766/
18. Guan W, Ni Z, Hu Y, Liang W, Ou C, He J, et al. Clinical Characteristics of Coronavirus Disease 2019 in China. N Engl J Med. 2020;382(18):1708-20. DOI: 10.1056/NEJMoa2002032.
19. Zhou F, Yu T, Du R, Fan G, Liu G, Liu Z, et al. Clinical course and risk factors for mortality of adult inpatients with COVID-19 in Wuhan, China: a retrospective cohort study. The Lancet [Internet].2020 [citado 06 Sep 2021];395:1054-62. Disponible en: https://www.thelancet.com/journals/lancet/article/PIIS0140-6736(20)30566-3/fulltext
20. Ghinai I, McPherson TD, Hunter JC, Kirking HL, Christiansen D, Joshi K, et al. First known person-to-person transmission of severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) in the USA. Lancet [Internet]. 2020 Abr [citado 06 Sep 2021];395(10230):1137-44. Disponible en: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7158585/
21. Sun K, Chen J, Viboud C. Early epidemiological analysis of the coronavirus disease 2019 outbreak based on crowdsourced data: a population-level observational study. Lancet [Internet]. 2020 Feb [citado 06 Sep 2021];2(4):e201-08. Disponible en: https://www.thelancet.com/journals/landig/article/PIIS2589-7500(20)30026-1/fulltext
22. Madjid M, Safavi-Naeini P, Solomon SD, Vardeny O. Potential. Effects of Coronaviruses on the Cardiovascular System A Review. JAMA Cardiol [Internet]. 2020 Jul [citado 06 Sep 2021];15(7):831-40. Disponible en: https://pubmed.ncbi.nlm.nih.gov/32219363/
Published
How to Cite
Issue
Section
License
Copyright (c) 2022 Yoan Pérez-Ojeda, Mildrey Jiménez-López, Carlos Jorge Hidalgo-Mesa, María Obdulia Benítez-Pérez, Juan Carlos Ojeda-Blanco, Lesvy Mendoza-Cabrera

This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License.
Copyright: Camagüey Medical Archive Magazine, offers immediately after being indexed in the SciELO Project; Open access to the full text of the articles under the principle of making available and free the research to promote the exchange of global knowledge and contribute to a greater extension, publication, evaluation and extensive use of the articles that can be used without purpose As long as reference is made to the primary source.
Conflicts of interest: authors must declare in a mandatory manner the presence or not of conflicts of interest in relation to the investigation presented.
(Download Statement of potential conflicts of interest)
The Revista Archivo Médico de Camagüey is under a License Creative Commons Attribution-Noncommercial-No Derivative Works 4.0 International (CC BY 4.0).
This license allows others to distribute, to mix, to adjust and to build from its work, even for commercial purposes, as long as it is recognized the authorship of the original creation. This is the most helpful license offered. Recommended for maximum dissemination and use of licensed materials. The full license can be found at: https://creativecommons.org/licenses/












 22 julio 2025
22 julio 2025