Epidemiological characteristics of supracondylar fractures of the humerus in children and adolescents
Abstract
Introduction: Traumatic injuries of the elbow are very frequent, some of them are difficult to treat and are associated with complications, of which supracondylar fractures of the humerus are one of the most frequent.
Objective: To describe the epidemiological behavior of a group of patients with this traumatic disease.
Methods: A descriptive observational study was carried out in patients treated at the Dr. Eduardo Agramonte Piña Provincial Pediatric Hospital in the city of Camagüey from January 1st, 2018 to December 31st, 2021 with a total of 48 months.
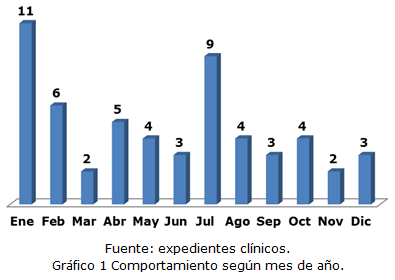
Results: the male-female sex ratio of the 56 patients was 3.3 to 1, the left-right elbow was 1.9 to 1, and the urban rural area was 2.2 to 1. The average age in general was 7.5 years. The average hospital stay was 4.8 days. The extension mechanism was the most frequent finding, as well as grade III fractures. The months of January and July together with the days of Thursday, Friday and Sunday are the ones with the largest number of patients. Closed reduction and percutaneous fixation with Kirschner wires was the most used method in this traumatic entity.
Conclusions: Supracondylar fractures of the humerus in children are more frequent in males and in the left elbow. The average age of males is higher than that of females. Rural areas provide the largest number of patients. The most used treatment is surgery and immediate complications are infrequent.
DeCS: HUMERAL FRACTURES; ELBOW JOINT/injuries; BONE WIRES; OPEN FRACTURE REDUCTION; CLOSED FRACTURE REDUCTION.
Downloads
References
1. Ho C. Upper Extremity Injuries. En: Herring JA. Tachdjian's Pediatric Orthopaedics. 6th ed. Philadelphia: Elsevier; 2020. p. 1191-1216.
2. Sawyer JR, Spence DD. Fractures and Dislocations in Children. En: Azar FM, Beaty JH. Campbell's Operative Orthopaedics. 14th ed. Philadelphia: Elsevier; 2021. p. 1502-1509.
3. Ausó-Pérez JR, Rodríguez-Blanes GM. Comprehensive Analysis of Pediatric Supracondylar Fractures in the Emergency Department; A Single Center Experience. Bull Emerg Trauma [Internet]. 2020 Jul [citado 12 Jun 2022];8(3):142-47. Disponible en: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7468217/
4. Challa S, Agarwal-Harding KJ, Levy P, Barr-Walker J, Sabatini CS. Supracondylar humerus fractures in low- and lower middle-income countries: a scoping review of the current epidemiology, treatment modalities, and outcomes. Int Orthop [Internet]. 2020 Nov [citado 12 Jun 2022];44(11):2443-2448. Disponible en: https://pubmed.ncbi.nlm.nih.gov/32691122/
5. Yuce A, Buyukkurt CD, Karslioglu B, Oncul A, Yerli M, Gurbuz H. Does Localisation of Fracture Line, According to Epicondyles, Affect Ligamentotaxis Negatively in Displaced Pediatric Supracondylar Humerus Fractures? J Coll Physicians Surg Pak [Internet]. 2021 [citado 12 Jun 2022];31(1):45-50. Disponible en: https://jcpsp.pk/oas/mpdf/generate_pdf.php?string=c0lEZnppTGN0V3JMZGFRWkR2NVBGZz09
6. Shenoy PM, Islam A, Puri R. Current Management of Paediatric Supracondylar Fractures of the Humerus. Cureus [Internet]. 2020 May [citado 12 Jun 2022];12(5):e8137. Disponible en: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7294900/
7. Aparicio Martínez JL, Pino Almero L, Cibrian Ortiz de Anda RM, Guillén Botaya E, García Montolio M, Mínguez Rey MF. Epidemiological study on supracondylar fractures of distal humerus in pediatric patients. Rev Esp Cir Ortop Traumatol [Internet]. 2019 Nov-Dic [citado 12 Jun 2022];63(6):394-399. Disponible en: https://pubmed.ncbi.nlm.nih.gov/31521582/
8. Eguia FA, Gottlich CP, Vora M, Klyce W, Hassan S, Sponseller PD, et al. Radiographic assessments of pediatric supracondylar fractures and mid-term patient-reported outcomes. Medicine [Internet]. 2020 Oct [citado 12 Jun 2022];99(41):e22543. Disponible en: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7544399/
9. Bekmez S, Camp MW, Ling R, El-Amiri N, Howard AW. Supracondylar Humerus Fractures in Older Children: Success of Closed Reduction and Percutaneous Pinning. J Pediatr Orthop [Internet]. 2021 Abr [citado 12 Jun 2022];41(4):242-248. Disponible en: https://pubmed.ncbi.nlm.nih.gov/33655902/
10. Ejagwulu FS, Amaefule KE, Dahiru IL, Aniko I, Ejagwulu EE. Challenges in the management of supracondylar humeral fractures in children in resource-constrained settings. West Afr J Med [Internet]. 2021 Sep [citado 12 Jun 2022];38(9):[aprox. 7 p.]. Disponible en: https://pubmed.ncbi.nlm.nih.gov/34677170/
11. Egol KA, Koval KJ, Zuckerman JD. Handbook of Fracture. 6th ed. Philadelphia: Wolter Kluwer; 2019.
12. LiBrizzi CL, Klyce W, Ibaseta A, Shannon C, Lee RJ. Sex-based differences in pediatric supracondylar humerus fractures. Medicine [Internet]. 2020 May [citado 12 Jun 2022];99(20):e20267. Disponible en: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7253849/
13. Mansor Y, Givon A, Sherr-Lurie N, Seltser A, Schindler A, Givon U. Is a radiograph needed one week after internal fixation of a supracondylar humeral fracture? J Pediatr Orthop B [Internet]. 2019 Nov [citado 12 Jun 2022];28(6):[aprox. 5 p.]. Disponible en: https://pubmed.ncbi.nlm.nih.gov/31361706/
14. Baidoo PK, Kumah-Ametepey R, Segbefia M, Buunaaim ADB. Treatment and outcomes of pediatric supracondylar humeral fractures in Korle Bu Teaching Hospital. OTA Int [Internet]. 2021 Jun [citado 12 Jun 2022];4(2):e124. Disponible en: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC8568478/
15. Anjum R, Sharma V, Jindal R, Singh TP, Rathee N. Epidemiologic pattern of paediatric supracondylar fractures of humerus in a teaching hospital of rural India: a prospective study of 263 cases. Chin J Traumatol [Internet]. 2017 Jun [citado 12 Jun 2022];20(3):158-160. Disponible en: https://pubmed.ncbi.nlm.nih.gov/28511800/
16. Rokaya PK, Karki DB, Rawal M, Limbu D, Menyangbo S, Devkota H. Pattern of Pediatric Supracondylar Fracture Operated at A Rural Teaching Hospital of Nepal: A Descriptive Cross-sectional Study. JNMA J Nepal Med Assoc [Internet]. 2020 Mar [citado 12 Jun 2022];58(223):153-157. Disponible en: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7580320/
17. Kitta MI, Ismiarto YD, Saleh MR, Sakti M, Abidin MA, Putra LT. Analysis of radiological alignment and functional outcomes of pediatric patients after surgery with displaced supracondylar humerus fracture: a cross sectional study. Int Journal Surg Open [Internet]. 2020 [citado 12 Jun 2022];24:[aprox. 6 p.]. Disponible en: https://doi.org/10.1016/j.ijso.2020.05.011
18. Kapicioglu M, Erden T, Agir M, Küçükdurmaz F. The reliability of use of WhatsApp in type 1 and type 2 pediatric supracondylar fractures. Eklem Hastalik Cerrahisi [Internet]. 2019 [citado 12 Jun 2022];30(2):149-154. Disponible en: https://pubmed.ncbi.nlm.nih.gov/31291864/
19. Marengo L, Cravino M, Origo C. Practices concerning management of Gartland type III supracondylar humeral fractures among Italian pediatric orthopedic surgeons. J Pediatr Orthop B [Internet]. 2019 [citado 12 Jun 2022];28(3):[aprox. 3 p.]. Disponible en: https://pubmed.ncbi.nlm.nih.gov/30920438/
20. Striano BM, De Mattos C, Ramski DE, Flynn KR, Horn BD. Displaced supracondylar humerus fractures in toddlers. Orthopedics [Internet]. 2020 Sep [citado 12 Jun 2022];43(5):[aprox. 3 p.]. Disponible en: https://pubmed.ncbi.nlm.nih.gov/32602923/
21. Schroeder NO, Seeley MA, Hariharan A, Farley FA, Caird MS, Li Y. Utility of Postoperative Antibiotics After Percutaneous Pinning of Pediatric Supracondylar Humerus Fractures. J Pediatr Orthop [Internet]. 2017 Sep [citado 12 Jun 2022];37(6):363-367. Disponible en: https://pubmed.ncbi.nlm.nih.gov/26558958/
22. Guo M, Xie Y, Su Y. Open Reduction of Neglected Supracondylar Humeral Fractures With Callus Formation in Children. J Pediatr Orthop [Internet]. 2020 Sep [citado 12 Jun 2022];40(8):e703-e707. Disponible en: https://pubmed.ncbi.nlm.nih.gov/32011548/
23. Duffy S, Flannery O, Gelfer Y, Monsell F. Overview of the contemporary management of supracondylar humeral fractures in children. Eur J Orthop Surg Traumatol [Internet]. 2021 [citado 12 Jun 2022];31(5):871-881. Disponible en: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC8233294/
24. Hockensmith LH, Muffly BT, Wattles MR, Snyder EN, McFarland BJ, Jacobs C, et al. Evaluating Perioperative Complications Surrounding Supracondylar Humerus Fractures: Expanding Indications for Outpatient Surgery. J Pediatr Orthop [Internet]. 2021 Oct [citado 12 Jun 2022];41(9):e745-e749. Disponible en: https://pubmed.ncbi.nlm.nih.gov/34354025/
25. Armstrong DG, Monahan K, Lehman EB, Hennrikus WL. The Pediatric Open Supracondylar Fracture: Associated Injuries and Surgical Management. J Pediatr Orthop [Internet]. 2021 Abr [citado 12 Jun 2022];41(4):e342-e346. Disponible en: https://pubmed.ncbi.nlm.nih.gov/33560707/
26. Ozcan M, Altinoz O, Erem M, Ciftdemir M, Copuroglu C, Turan FN. Prognosis and risk factors of nerve injuries in displaced pediatric supracondylar humerus fractures. Niger J Clin Pract [Internet]. 2020 May [citado 12 Jun 2022];23(5):647-653. Disponible en: https://pubmed.ncbi.nlm.nih.gov/32367871/
Published
How to Cite
Issue
Section
License
Copyright (c) 2022 Alejandro Alvarez-López, Valentina Valdebenito-Aceitón, Sergio Ricardo Soto-Carrasco, Daniel Serrano-González, Yenima de la Caridad García-Lorenzo

This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License.
Copyright: Camagüey Medical Archive Magazine, offers immediately after being indexed in the SciELO Project; Open access to the full text of the articles under the principle of making available and free the research to promote the exchange of global knowledge and contribute to a greater extension, publication, evaluation and extensive use of the articles that can be used without purpose As long as reference is made to the primary source.
Conflicts of interest: authors must declare in a mandatory manner the presence or not of conflicts of interest in relation to the investigation presented.
(Download Statement of potential conflicts of interest)
The Revista Archivo Médico de Camagüey is under a License Creative Commons Attribution-Noncommercial-No Derivative Works 4.0 International (CC BY 4.0).
This license allows others to distribute, to mix, to adjust and to build from its work, even for commercial purposes, as long as it is recognized the authorship of the original creation. This is the most helpful license offered. Recommended for maximum dissemination and use of licensed materials. The full license can be found at: https://creativecommons.org/licenses/












 22 julio 2025
22 julio 2025