Second trimester fetal biometry: predicting small and large births for gestational age
Abstract
Introduction: Medical biometrics has made it possible to identify predictive variables of birth weight.
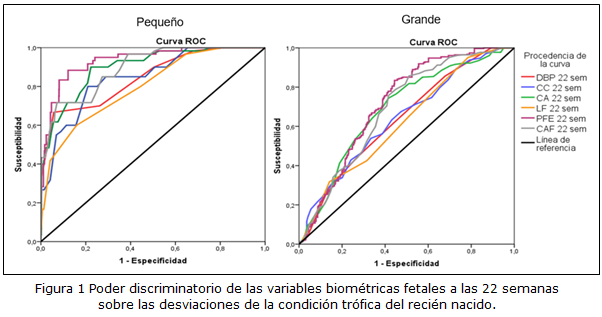
Objective: To determine the local discriminatory power and performance of fetal biometric variables at 22 weeks on the trophic condition of the newborn.
Methods: An observational, analytical and retrospective study was carried out in three health areas of the Santa Clara municipality, in the period between January 2013 and December 2019. From a population of 6,035 births, 2,454 were selected by simple random sampling. Data were obtained from records of genetic consultations. In the analysis, areas under the Receiver Operating Characteristic curve were constructed and performance indicators for diagnostic tests were calculated.
Results: The areas under the curve of the biometric variables discriminate those born small and large for gestational age. In the small ones they exceed 0.840 except for the length of the femur; in the large ones, the estimated fetal weight reaches a curve of 0.715, the rest are lower. Local cut-off points are estimated. The performance indicators of the biometrics maintain a regular behavior; those that are estimated by transforming the values from the reference tables are more specific with values above 80%; while those calculated after transforming the variables by the estimated cut-off points raise the sensitivity above 60%.
Conclusions: All biometric variables have discriminatory capacity for deviations of the trophic condition at birth, preferably for small births for gestational age. The optimal cut-off points identified differ from those established in the reference tables. The performance indicators of the fetal biometric variables showed superiority according to the estimated cut-off points with respect to those of the reference tables.
DeCS: BIOMETRY; FETAL WEIGHT; GESTATIONAL AGE; SAGITTAL ABDOMINAL DIAMETER; BIRTH WEIGHT.
Downloads
References
1. Moreno-Fernandez J, Ochoa JJ, Lopez-Frias M, Díaz-Castro J. Impact of Early Nutrition, Physical Activity and Sleep on the Fetal Programming of Disease in the Pregnancy: A Narrative Review. Nutrients [Internet]. 2020 Dic [citado 03 Nov 2022];12(12):3900. Disponible en: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7766505/
2. Freire Carrera MA, Alvarez Ochoa R, Vanegas Izquierdo PE, Peña Cordero SJ. Bajo peso al nacer: Factores asociados a la madre. Revista Científica y Tecnológica UPSE [Internet]. 2020 [citado 03 Nov 2022];7(2):01-8. Disponible en: https://incyt.upse.edu.ec/ciencia/revistas/index.php/rctu/article/view/527/478
3. World Health Organization. WHO Global status report on alcohol and health 2018 [Internet]. Geneva: WHO; 2018 [citado 03 Nov 2022]. Disponible en: https://www.mhinnovation.net/resources/who-global-status-report-alcohol-and-health-2018
4. Ministerio de Salud Pública. Programa Nacional de Atención Materno Infantil 1999 [Internet]. La Habana: Minsap; 2012 [citado 03 Nov 2022]. Disponible en: https://files.sld.cu/sida/files/2012/01/programa-nacional-de-atencion-materno-infantil-1999.pdf
5. Aggarwal N, Sharma GL. Fetal ultrasound parameters: Reference values for a local perspective. Indian J Radiol Imaging [Internet]. 2020 Abr-Jun [citado 03 Nov 2022];30(2):149-55. Disponible en: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7546290/
6. Campbell S, Wilkin D. Ultrasonic measurement of fetal abdomen circumference in the estimation of fetal weight. Br J Obstet Gynecol. 1975 Sep;82(9):689-97.
7. Hiersch L, Melamed N. Fetal growth velocity and body proportion in the assessment of growth. Am J Obstet Gynecol [Internet]. 2018 Feb [citado 03 Nov 2022];218(2):S700-S11. Disponible en: https://www.ajog.org/article/S0002-9378(17)32489-4/pdfSummary
8. Sosa-Olavarría A, Álvarez-Moya E, Schenone Giugni MH, Pianigiani Edgardo C, Zurita-Peralta J, Schenone Giugni CV. Índice cefálico/abdominal/femoral (C+AF), herramienta antropométrica efectiva en la evaluación del crecimiento fetal y de sus desviaciones. Rev peru ginecol obstet [Internet]. 2020 Oct-Dic [citado 03 Nov 2022];66(4). Disponible en: http://www.scielo.org.pe/scielo.php?script=sci_arttext&pid=S2304-51322020000400003
9. Montoya-Restrepo NE, Correa-Morales JC. Curvas de Peso al Nacer. Rev salud pública [Internet]. 2007 Ene-Mar [citado 03 Nov 2022];9(1). Disponible en: http://www.scielo.org.co/scielo.php?script=sci_arttext&pid=S0124-00642007000100003
10. Ferreiro RM, Valdés Amador L. Eficacia de distintas fórmulas ecográficas en la estimación del peso fetal a término. Rev cuba obstet ginecol [Internet]. 2010 [citado 03 Nov 2022];36(4):490-501. Disponible en: https://docplayer.es/32035413-Eficacia-de-distintas-formulas-ecograficas-en-la-estimacion-del-peso-fetal-a-termino.html
11. Armesto D, España B. Pruebas Diagnósticas: Curvas ROC. Electron J Biomed [Internet]. 2011 [citado 03 Nov 2022];1:77-82. Disponible en: https://biomed.uninet.edu/2011/n1/armesto.pdf
12. Kumar R, Indrayan A. Receiver operating characteristic (ROC) curve for medical researchers. Indian Pediatr [Internet]. 2011 Abr [citado 03 Nov 2022];48(4):277-87. Disponible en: https://link.springer.com/article/10.1007/s13312-011-0055-4
13. Asociación Médica Mundial. Declaración de Helsinki de la AMM-Principios éticos para las investigaciones médicas en seres humanos [Internet]. 2013 [citado 03 Nov 2022]. Disponible en: http://www.redsamid.net/archivos/201606/2013-declaracion-helsinki-brasil.pdf
14. Águila Setién S, Delgado Calzado JJ, Breto García A, Cabezas Cruz E, Santisteban Alba S, et al. Consenso de Procederes diagnósticos y terapéuticos en Obstetricia y Perinatología. Ciudad de La Habana: MINSAP; 2010.
15. Álvarez-Guerra González E, Hernández Díaz D, Sarasa Muñoz NL, Barreto Fiu EE, Limas Pérez Y, Cañizares Luna O. Biometría fetal: capacidad predictiva para los nacimientos grandes para la edad gestacional. Arch méd Camagüey [Internet]. 2017 [citado 03 Nov 2022];21(6):695-704. Disponible en: http://scielo.sld.cu/pdf/amc/v21n6/amc030617.pdf
16. Alvarez-Guerra González E, Hernández Díaz D, Sarasa Muñoz NL, Limas Pérez Y, Orosco Muñoz C, Artiles Santana A. Biometría fetal: capacidad predictiva para los nacimientos pequeños según su edad gestacional. Medicentro [Internet]. 2017 [citado 03 Nov 2022];21(2):112-9. Disponible en: http://www.medicentro.sld.cu/index.php/medicentro/article/view/2142/1943
17. Molina Hernández OR, Monteagudo Ruiz CL. Caracterización perinatal del recién nacido macrosómico. Rev cuba obstet ginecol [Internet]. 2010 Sep;36(3):313-21. Disponible en: http://scielo.sld.cu/pdf/gin/v36n3/gin02310.pdf
18. Hadlock FP, Deter RL, Harrist RB, Park S. Estimating fetal age: computer-assisted analysis of multiple fetal growth parameters. Radiology. 1984;152(2):497-501.
19. Nathan R, Savabi M, Beddow ME, Katukuri VR, Fritts CM, Izquierdo LA, et al. The Hadlock method is superior to newer methods for the prediction of the birth weight percentile. J Ultrasound Med [Internet]. 2019 Mar [citado 03 Nov 2022];38(3):587-96. Disponible en: https://onlinelibrary.wiley.com/doi/abs/10.1002/jum.14725
20. Wanyonyi S, Orwa J, Ozelle H, Martínez J, Atsali E, Vinayak S, et al. Routine third‐trimester ultrasound for the detection of small‐for‐gestational age in low‐risk pregnancies (ROTTUS study): randomized controlled trial. Ultrasound Obstet Gynecol [Internet]. 2021 Jun [citado 03 Nov 2022];57(6):910-16. Disponible en: https://pubmed.ncbi.nlm.nih.gov/33619823/
21. Corley Price R, Roeckner J, Odibo L, Odibo A. Comparing fetal biometric growth velocity versus estimated fetal weight for prediction of neonatal small for gestational age. J Matern Fetal Neonatal Med [Internet]. 2022 Oct [citado 03 Nov 2022];35(20):3931-36. Disponible en: https://www.tandfonline.com/doi/abs/10.1080/14767058.2020.1844652
22. Moraitis AA, Shreeve N, Sovio U, Brocklehurst P, Heazell AEP, Thornton JG, et al. Universal third-trimester ultrasonic screening using fetal macrosomia in the prediction of adverse perinatal outcome: A systematic review and meta-analysis of diagnostic test accuracy. PLoS Med [Internet]. 2020 Oct [citado 03 Nov 2022];17(10):e1003190. Disponible en: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7553291/
23. Roeckner JT, Odibo L, Odibo AO. The value of fetal growth biometry velocities to predict large for gestational age (LGA) infants. J Matern Fetal Neonatal Med [Internet]. 2022 Jun [citado 03 Nov 2022];35(11):2099-2104. Disponible en: https://pubmed.ncbi.nlm.nih.gov/32546027/
24. Monier I, Ego A, Benachi A, Hocquette A, Blondel B, Goffinet F, et al. Comparison of the performance of estimated fetal weight charts for the detection of small‐and large‐for‐gestational age newborns with adverse outcomes: a French population‐based study. BJOG [Internet]. 2021 Nov [citado 03 Nov 2022];129(6):938-48. Disponible en: https://europepmc.org/article/med/34797926
Published
How to Cite
Issue
Section
License
Copyright (c) 2022 Elizabeth Álvarez-Guerra-González, Nélida Liduvina Sarasa-Muñoz, Oscar Cañizares-Luna, Celidanay Ramírez-Mesa, Disney Borrego-Gutiérrez, Alina Artiles-Santana

This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License.
Copyright: Camagüey Medical Archive Magazine, offers immediately after being indexed in the SciELO Project; Open access to the full text of the articles under the principle of making available and free the research to promote the exchange of global knowledge and contribute to a greater extension, publication, evaluation and extensive use of the articles that can be used without purpose As long as reference is made to the primary source.
Conflicts of interest: authors must declare in a mandatory manner the presence or not of conflicts of interest in relation to the investigation presented.
(Download Statement of potential conflicts of interest)
The Revista Archivo Médico de Camagüey is under a License Creative Commons Attribution-Noncommercial-No Derivative Works 4.0 International (CC BY 4.0).
This license allows others to distribute, to mix, to adjust and to build from its work, even for commercial purposes, as long as it is recognized the authorship of the original creation. This is the most helpful license offered. Recommended for maximum dissemination and use of licensed materials. The full license can be found at: https://creativecommons.org/licenses/












 22 julio 2025
22 julio 2025