Congenital chylothorax in an extreme preterm newborn
Abstract
Introduction: Congenital chylothorax is a rare respiratory disease; however, it is the most common cause of pleural effusion in live newborns.
Objective: To present a case of congenital chylothorax as an uncommon cause of respiratory distress in a newborn treated at the Gyneco-Obstetric Hospital of Villa Clara.
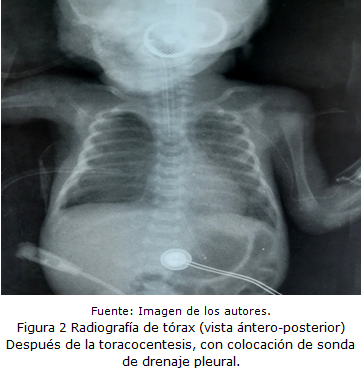
Case report: Male patient, who was born at 26.2 weeks of gestational age, by eutocic delivery, with membrane time rupture of an hour, meconium amniotic fluid, to whom was given an Apgar score of 7/8 (normal) and a birth weight of 950 grams; with diagnose of connatal sepsis was necessary to treat with mechanical ventilation. At six days of age presented a clinical deterioration, with decrease of the vesicular murmur in the right hemithorax and at chest X-ray was observed a veiled right lung. The chest ultrasound confirmed a right pleural effusion that was punctured and the study of the drained fluid showed characteristics of a chylothorax. Conservative treatment was indicated (with complete parenteral feeding: traximin without lipid intake) and subsequently with milk rich in short and medium chain fatty acids (Enfaport® from Nestlé Company). Breastmilk was incorporated 15 days after the diagnose. He required prolonged mechanical ventilation. With a satisfactory evolution, he was discharged from the hospital center.
Conclusions: The resolution of this entity is achieved through conservative treatment, without the presence of recurrence.
DeCS: CHYLOTHORAX/genetics; INFANT, PREMATURE; PLEURAL EFFUSION; RESPIRATORY DISTRESS SYNDROME, NEWBORN; RESPIRATION, ARTIFICIAL.
Downloads
References
1. Antón JL, Luna MC, Gimeno A. Derrame pleural no paraneumónico, quilotórax, hemotórax y mediastinitis. Protoc diagn ter pediatr [Internet]. 2017 [citado 01 Mar 2022];1:211-219. Disponible en: https://www.aeped.es/sites/default/files/documentos/13_derrame_pleural.pdf
2. Lima AL, Tresoldi M, Ramos CD, de Melo Alexandre A, Mendes R, Appenzeller S, et al. Quilotórax bilateral espontâneo apôs vômitos excessivos em criança. Rev Paul Pediatr [Internet]. 2016 [citado 04 Feb 2019];34(2):518-21. Disponible en: https://www.academia.edu/58800410/Quilotórax_bilateral_espontâneo_após_vômitos_excessivos_em_criança
3. Fuentes MJ, Novoa J, Contreras I, Vega Briceño L. Quilotórax congénito: una causa rara de distres neonatal. Reporte de caso. Neumo pediátr [Internet]. 2010 [citado 25 Feb 2019];5(2):104-8. Disponible en: https://www.neumologia-pediatrica.cl/PDF/201052/quilotorax.pdf
4. Roehr CC, Jung A, Proquitté H, Blankenstein O, Hammer H, Lakhoo K, et al. Somatostatin or octreotide as treatment options for chylothorax in young children: a systematic review. Intensive Care Med [Internet]. 2006 [citado 01 Mar 2022];32(5):650-7. Disponible en: https://link.springer.com/article/10.1007/s00134-006-0114-9
5. Salgado Andino CA. Tratamiento conservador del quilotórax posquirúrgico en paciente pediátrico. Cambios [Internet]. 2021 [citado 01 Mar 2022];20(1):94-8. Disponible en: https://revistahcam.iess.gob.ec/index.php/cambios/article/view/524/447
6. Büttiker V, Fanconi S, Burger R. Chylothorax in children. Guidelines for diagnosis and management. Anionic Chest [Internet]. 1999 [citado 29 Ene 2022];116(3):682-7. Disponible en: https://doi.org/10.1378/chest.116.3.682
7. Church J, Antunez A, Dean A, Deatrick K, Attar M, Gadepalli S. Evidence-based management of chylothorax in infants. J Pediatr Surg [Internet]. 2017 [citado 27 Feb 2022];52(6):907-12. Disponible en: https://doi.org/10.1016/j.jpedsurg.2017.03.010
8. Christofe N, Ximenes C. Incidence and Treatment of Chylothorax in Children Undergoing Corrective Surgery for Congenital Heart Diseases. Braz J Cardiovasc Surg [Internet]. 2017 [citado 28 Ene 2022];32(5):390-3. Disponible en: https://www.doi.org/10.21470/1678-9741-2017-0011.
9. Meizoso AI, Cervantes M, Rodríguez LA. Quilotórax neonatal. MediCiego [Internet]. 2017 [citado 01 Mar 2022];23(4):[aprox. 5 p.] Disponible en: https://www.revmediciego.sld.cu/index.php/mediciego/article/view/826/1169
10. Aguilar López LA, Rodríguez Moncada LL, Díaz Díaz AM, Peinado Acevedo JS. Recién nacido prtérmino con quilotórax congénito bilateral, una entidad infrecuente que amenaza la vida. MÉD UIS [Internet]. 2017 [citado 01 Mar 2022];30(1):87-92. Disponible en: https://revistas.uis.edu.co/index.php/revistamedicasuis/article/view/6311/6539
11. Huamán Rodríguez MR, Malca Suarez RM, Peralta Chávez V, Aguilar Urbina EW. Quilotórax congénito en prematuro tardío: reporte de caso. Rev méd Trujillo [Internet]. 2019 [citado 31 Ene 2022];14(2):209-13. Disponible en: http://dx.doi.org/10.17268/rmt.2019.v14i04.08
Published
How to Cite
Issue
Section
License
Copyright (c) 2022 Lil Katia Rodríguez-Díaz, Ana Miriam Clemades-Méndez, Seydis Chaviano-Rodríguez, Eduardo Augusto Kedisobua-Clemades

This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License.
Copyright: Camagüey Medical Archive Magazine, offers immediately after being indexed in the SciELO Project; Open access to the full text of the articles under the principle of making available and free the research to promote the exchange of global knowledge and contribute to a greater extension, publication, evaluation and extensive use of the articles that can be used without purpose As long as reference is made to the primary source.
Conflicts of interest: authors must declare in a mandatory manner the presence or not of conflicts of interest in relation to the investigation presented.
(Download Statement of potential conflicts of interest)
The Revista Archivo Médico de Camagüey is under a License Creative Commons Attribution-Noncommercial-No Derivative Works 4.0 International (CC BY 4.0).
This license allows others to distribute, to mix, to adjust and to build from its work, even for commercial purposes, as long as it is recognized the authorship of the original creation. This is the most helpful license offered. Recommended for maximum dissemination and use of licensed materials. The full license can be found at: https://creativecommons.org/licenses/












 22 julio 2025
22 julio 2025