Survival after liver transplantation in recipients with biliary complications
Abstract
Introduction: Complications related to biliary anastomosis are recognized as the first cause of post-liver transplantation morbidity and can negatively affect patient survival.
Objective: To evaluate the behavior of long-term survival in patients with post-transplant biliary complications.
Methods: An observational, longitudinal, and retrospective study was carried out in 152 patients with liver transplantation between 1999-2019, the following were excluded: patients with survival less than 72 hours, retransplants and patients with hepatic artery thrombosis. The variables studied were age and sex of the recipients, pre-transplant etiology, MELD index (Model for End Stage Liver Desease), biliary anastomosis technique, type of biliary complication, time of onset and treatment used. The categorical variables were related using the Chi square statistical test and Fisher's exact test, with significant differences when p
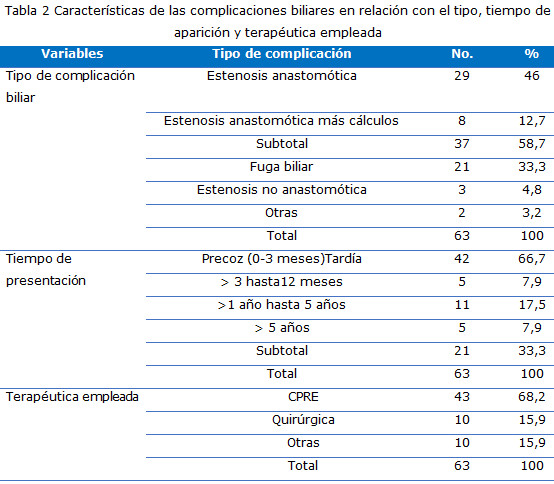
Results: They were significantly related to the presence of biliary complication, a higher MELD index score (p = 0.008) and the end-to-end anastomosis technique (p = 0.039). Early biliary complications (66.7%) and anastomotic stenosis (58.7%) predominated. Treatment by endoscopic retrograde cholangiopancreatography (ERCP) was the most used (68.2%). Patients with biliary complications had a mean survival of 10.9 years (95% CI 8.75-13.19), while patients without it had a mean of 9 years (95% CI 7.03 -10.98); there was no significant difference (p = 0.24).
Conclusions: Biliary complications were an important cause of post-transplant morbidity, but without affecting patient survival.
DeCS: LIVER TRANSPLANT; BILIARY TRACT DISEASES/complications; SURVIVAL; SURGICAL ANASTOMOSIS; MORBIDITY.
Downloads
References
1. Duffy JP, Kao K, Ko CY, Farmer DG, McDiarmid SV, Hong JC, et al. Long-term patient outcome and quality of life after liver transplantation: analysis of 20-year survivors. Ann Surg [Internet]. 2010 [citado 18 May 2020];20(8):[aprox. 10 p.]. Disponible en: https://pubmed.ncbi.nlm.nih.gov/20881772/.
2. Charlton MR. Roadmap for improving patient and graft survival in the next 10 years. Liver Transpl [Internet]. 2016 [citado 26 May 2020];[aprox. 8 p.]. Disponible en: https://aasldpubs.onlinelibrary.wiley.com/doi/10.1002/lt.24602
3. Müller P, Kabacam G, Vibert E, Germani G, Petrowsky H. Current status of liver transplantation in Europe. Int J Surg [Internet]. 2020 Oct [citado 26 May 2020];82S:[aprox. 7 p.]. Disponible en: https://pubmed.ncbi.nlm.nih.gov/32454252/.
4. Boeva I, Karagyozov PI, Tishkov I. Post-liver transplant biliary complications: Current knowledge and therapeutic advances. World J Hepatol [Internet]. 2021 [citado 26 May 2020];22(S1):[aprox. 8 p.]. Disponible en: https://pubmed.ncbi.nlm.nih.gov/33584987/.
5. Kienlein S, Schoening W, Andert A, Kroy D, Neumann UP, Schmeding M. Biliary complications in liver transplantation. Impact of anastomotic technique and ischemic time on short- and long-term outcome. World J Transplant [Internet]. 2015 [citado 13 May 2020];5(4):[aprox. 10 p.]. Disponible en: https://pubmed.ncbi.nlm.nih.gov/26722658/.
6. Karimian N, Westerkamp AC, Porte RJ. Biliary complications after orthotropic liver transplantation. Curr Opin Organ Trans¬plant [Internet]. 2014 [citado 13 May 2020];19:[aprox. 8 p.]. Disponible en: https://pubmed.ncbi.nlm.nih.gov/24752062/.
7. Kaltenborn A, Gutcke A, Gwiasda J, Klempnauer J, Schrem H. Biliary complications following liver transplantation: Single center experience over three decades and recent risk factors. World J Hepatol [Internet]. 2017 [citado 13 May 2020];9(3):[aprox. 8 p.]. Disponible en: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5295148/.
8. Mejía GA, Olarte-Parra C, Pedraza A, Rivera JB, Benavides CA. Biliary Complications After Liver Transplantation: Incidence, Risk Factors and Impact on Patient and Graft Survival. Transpl Proceed [Internet]. 2016 [citado 4 Jun 2020];48:[aprox. 4 p.]. Disponible en: http://dx.doi.org/10.1016/j.transproceed.2016.02.033
9. Ma MX, Jayasekeran V, Chong AK. Benign biliary structures: prevalence, impact, and management strategies. Clin Exp Gastroenterol [Internet]. 2019 [citado 4 Jun 2020];26:[aprox. 4 p.]. Disponible en: https://www.dovepress.com/benign-biliary-strictures-prevalence-impact-and-management-strategies-peer-reviewed-fulltext-article-CEG
10. Rönning J, Berglund E, Arnelo U, Ericzon BG, Greg Nowak. Long-term Outcome of Endoscopic and Percutaneous Transhepatic Approaches for Biliary Complications in Liver Transplant Recipients. Transplantation Direct [Internet]. 2019 [citado 25 Feb 2019];5:e432. Disponible en: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6411220/.
11. Faleschini G, Vadal? di Prampero SF, Bulajic M, Baccarani U, Toniutto P, Panic N, et al. Predictors of endoscopic treatment outcome in the management of biliary complications after orthotopic liver transplantation, European. J Gastr Hepatol [Internet]. 2015 [citado 4 Feb 2018];27:[aprox. 5 p.]. Disponible en: https://pubmed.ncbi.nlm.nih.gov/25486026/.
12. Lima AS, Pereira BB, Jungmann S, Machado CJ, Correia MD. Risk factors for post-liver transplant biliary complications in the absence of arterial complications. ABCD Arq Bras Cir Dig [Internet]. 2020 [citado 25 Feb 2019];33(3):e1541. Disponible en: https://doi.org/10.1590/0102-672020200003e1541
13. Coelho J LL, Molena A, Freitas A, Matias J. Biliary Complications after Liver Transplantation. ABCD Arq Bras Cir Dig [Internet]. 2017 [citado 3 Mar 2020];30:[aprox. 5 p.]. Disponible en:
https://www.researchgate.net/publication/318872370
14. Gabrielli M, Norero E, Figueroa E, Cortés P, Pimentel F, Huete Á, et al. Incidencia, factores de riesgo y tratamiento de las complicaciones biliares del trasplante hepático. Rev Chil Cir [Internet]. 2010 [citado 3 Mar 2020];62:[aprox. 7 p.]. Disponible en: http://dx.doi.org/10.4067/S0718-40262010000400006
15. Kaldas FM, Korayem IM, Russell TA, Agopian VG, Aziz A, Di Norcia J, et al. Assessment of Anastomotic Biliary Complications in Adult Patients Undergoing High-Acuity Liver Transplant. JAMA Surg [Internet]. 2019 [citado 26 Jun 2020];154:[aprox. 9 p.]. Disponible en: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6537782/.
16. Qian YB, Liu CL, Lo CM, Fan ST. Risk factors for biliary complications after liver transplantation. Arch Surg [Internet]. 2004 Oct [citado 26 Junio 2020];139(10):[aprox. 5 p.]. Disponible en: https://pubmed.ncbi.nlm.nih.gov/15492152/.
17. Akamatsu N, Sugawara Y, Hashimoto D. Biliary reconstruction, its complications and management of biliary complications after adult liver transplantation: a systematic review of the incidence, risk factors and outcome. Transpl Int [Internet]. 2011 [citado 12 Ago 2020];24:[aprox. 14 p.]. Disponible en: https://onlinelibrary.wiley.com/doi/full/10.1111/j.1432-2277.2010.01202.x
18. Zhao JZ, Qiao LL, Du ZQ, Zhang J, Wang MZ. T-tube vs. no T-tube for biliary tract reconstruction in adult orthotopic liver transplantation: An updated systematic review and meta-analysis. World J Gastroent [Internet]. 2021 [citado 12 Ago 2020];27:[aprox. 15 p.]. Disponible en: https://doi.org/10.3748/wjg.v27.i14.1507
19. Moy BT, Birk JW. A Review on the Management of Biliary Complications after Orthotopic Liver Transplantation. J Clin Transl Hepatol [Internet]. 2019 [citado 9 May 2020];7:[aprox. 10 p.]. Disponible en: https://doi.org/10.14218/JCTH.2018.00028
20. Ram Mohan A, Govil S, Varghese J, Kota V, Reddy MS, Rela M. Changing Pattern of Biliary Complications in an Evolving Liver Transplant Unit. Liver Transpl [Internet]. 2017 [citado 4 Oct 2020];23:[aprox. 9 p.]. Disponible en: https://pubmed.ncbi.nlm.nih.gov/28152569/.
21. Castaño Llano R, Vélez Ruiz MH, Restrepo Gutiérrez JC, Hoyos Duque SI, Guzmán Luna CE, Mena Hurtado Á, et al. Endoscopic management o fbiliary complications following ortho topic liver transplantation. Rev Colomb Gastroenterol [Internet]. 2012 [citado 4 Oct 2020];27:[aprox. 12 p.]. Disponible en: http://www.scielo.org.co/scielo.php?pid=S0120-99572012000300005&script=sci_arttext&tlng=en
22. Tingle SJ, Thompson ER, Ali SS, Figueiredo R, Hudson M, Sen G, et al. Risk factors and impact of early anastomotic biliary complications after liver transplantation: UK registry analysis. BJS Open [Internet]. 2021 Mar 5 [citado 4 Oct 2020];5:zrab019. Disponible en: https://pubmed.ncbi.nlm.nih.gov/33855363/.
Published
How to Cite
Issue
Section
License
Copyright (c) 2022 Sheyla Moret-Vara, Marcia Samada-Suárez, Lissette Chao-González, Julio César Hernández-Perera, Kenia Yunarkis Valenzuela-Aguilera, Lisset Barroso-Márquez

This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License.
Copyright: Camagüey Medical Archive Magazine, offers immediately after being indexed in the SciELO Project; Open access to the full text of the articles under the principle of making available and free the research to promote the exchange of global knowledge and contribute to a greater extension, publication, evaluation and extensive use of the articles that can be used without purpose As long as reference is made to the primary source.
Conflicts of interest: authors must declare in a mandatory manner the presence or not of conflicts of interest in relation to the investigation presented.
(Download Statement of potential conflicts of interest)
The Revista Archivo Médico de Camagüey is under a License Creative Commons Attribution-Noncommercial-No Derivative Works 4.0 International (CC BY 4.0).
This license allows others to distribute, to mix, to adjust and to build from its work, even for commercial purposes, as long as it is recognized the authorship of the original creation. This is the most helpful license offered. Recommended for maximum dissemination and use of licensed materials. The full license can be found at: https://creativecommons.org/licenses/












 22 julio 2025
22 julio 2025