Quality of life in children of the Cuban Cochlear Implant Program
Keywords:
Implantes Cocleares, Calidad de Vida, Categorías del Rendimiento Auditivo, CAP-IIAbstract
Background: the studies published on the results of the Cuban Cochlear Implants Program refer to audiological and surgical evaluations, lacking the dimension that knowing about the impact of cochlear implants on the quality of life of children and their family.
Objective: to determine the impact in the Cuban Cochlear Implants Program on the quality of life of children and their family.
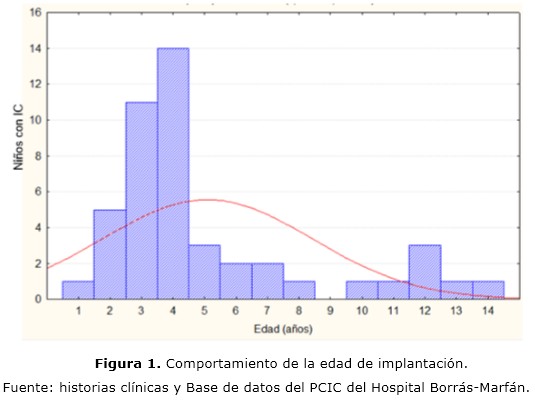
Methods: it was carried out a descriptive, prospective, longitudinal study (pre- and post-cochlear implant) from the application of a quality of life questionnaire of the international pediatric project cochlear pediatric implanted recipient observational study and the categories auditory performance test, being applied an analysis of variance of repeated measures.
Results: the study shows that cochlear implants impact on the quality of life of children and family, and improves significantly as early as six months post-cochlear implant, with greater benefits one year after implantation, supported by the findings of the categories auditory performance test. While parental expectations are adjusted as post-cochlear implant rehabilitation progresses.
Conclusions: cochlear implants impact on the quality of life of the child and family with the post-implant rehabilitation program progresses, adjusting the expectations of the parents or child's guardian, who report positive changes in the development of their daily activities, a sustained effect in the time.
DeCS: COCHLEAR IMPLANTS; HEARING LOSS; CHILD; QUALITY OF LIVE; HEALT PROGRAMS AND PLANS.
Downloads
References
1. Ching T, Dillon H, Leigh G, Cupples L. Learning from the Longitudinal Outcomes of Children with Hearing Impairment (LOCHI) study: summary of 5-year findings and implications. Int J Audiol. 2017;57(sup 2):S105-S111. doi:10.1080/14992027.2017.1385865
2. Pisoni DB, Kronenberger WG, Harris MS, Moberly AC. Three challenges for future research on cochlear implants. WJOHNS. 2017;3(4):240–254. doi:10.1016/j.wjorl.2017.12.010
3. Cupples L, Chin T, Bulton L, Leigh G, Marnane V, Whitfield J, et al. Language and speech outcomes of children with hearing loss and additional disabilities: Identifying the variables that influence performance at 5 years of age. Int J Audiol. 2018;57(Sup 2):S93–S104. doi:10.1080/14992027.2016.1228127
4. Wiseman KB, Warner-Czyz AD, Kwon S, Fiorentino K, Sweeney M. Relationships Between Daily Device Use and Early Communication Outcomes in Young Children With Cochlear Implants. Ear and Hearing Publish Ahead of Print. 2021.
doi: 10.1097/AUD.0000000000000999
5. Robles-Espinoza A, Rubio-Jurado B, De la Rosa-Galván E, Nava-Zavala A. Generalidades y conceptos de calidad de vida en relación con los cuidados de salud. El Residente [Internet]. 2016 [citado 19 Feb 2020];11:120-125. Disponible en: https://www.medigraphic.com/pdfs/residente/rr-2016/rr163d.pdf
6. Hinderink JB, Krabbe PF, Van Den Broek P. Development and application of a health-related quality-of-life instrument for adults with cochlear implants: the Nijmegen cochlear implant questionnaire. Otolaryngol Head Neck Surg. 2000;123(6):756-65. doi: 10.1067/mhn.2000.108203
7. Sanderson G, Ariyaratne T, Wyss J, Looi V. A global patient outcomes registry: Cochlear paediatric implanted recipient observational study (Cochlear™ P-IROS). BMC Ear Nose and Throat Disorders [Internet]. 2014 [citado 19 Feb 2020];14:10. Disponible en: https://bmcearnosethroatdisord.biomedcentral.com/articles/10.1186/1472-6815-14-10
8. Lenarz T, Muller L, Czerniejewska-Wolska H, Varela HV, Dotú CO, Durko M, et al. Patient-related benefits for adults with cochlear implantation: a multicultural longitudinal observational study. Audiol Neurotol. 2017;22(2):61-73. doi: 10.1159/000477533
9. Gaurav V, Sharma S, Singh S. Effects of Age at Cochlear Implantation on Auditory Outcomes in Cochlear Implant Recipient Children. Indian J Otolaryngol Head Neck Surg. 2019; 72(1):79-85. doi.org/10.1007/s12070-019-01753-4
10. Lenarz T. Cochlear implant-state of the art. GMS Curr Top Otorhinolaryngol Head Neck Surg. 2017;16:Doc04. doi:10.3205/cto000143
11. Manrique M, Ramos A, Vernetta C, Gil-Carcedo E, Lassaleta L, Sanchez-Cuadrado I, et al. Guía clínica sobre implantes cocleares. Acta Otorrinolaringol Esp. 2018. 70(1):47-54. doi.org/10.1016/j.otorri.2017.10.007.
12. Joint Committee on Infant Hearing (JCIH). Year 2019 Position Statement: Principles and Guidelines for Early Hearing Detection and Intervention Programs. The Journal of Early Hearing Detection and Intervention. 2019;4(2):1-44. doi 10.15142/fptk-b748
13. Núñez F, Jáudenes C, Sequí J, Vivanco A, Zubicaray J, Olleta I. Actualización de los programas de detección precoz de la sordera infantil: recomendaciones CODEPEH 2019 (Niveles 2, 3 y 4: diagnóstico, tratamiento y seguimiento. Rev Española de Discapacidad. 2020;8(I):219-246. doi.org/10.5569/2340-5104.08.01.13
14. Kim S, Lim EJ, Kim HS, Park JH, Jarng SS, Lee SH. Sex differences in a cross sectional study of age-related hearing loss in Korean. Clin Exp Otorhinolaryngol. 2010;3(1):27. doi 10.3342/ceo.2010.3.1.27
15. Raji A, Mounji H, Rochdi Y, Nouri H, Elfakiri M. Rehabilitation of hearing by cochlear implantation. J Nov Physiother Rehabil. 2019;3:082-086. doi: 10.29328/journal.jnpr.1001028
16. Sharma A, Dorman MF, Spahr AJ. A sensitive period for the development of the central auditory system in children with cochlear implants: implications for age of implantation. Ear Hear. 2002;23:532-539. doi: 10.1097/00003446-200212000-00004
17. Santiago-Pardo R, Benito-Orejas J, Sánchez-Rosso A, Rico-Paino M, Herrero-Galiacho A, Castro L. Selección de pruebas del lenguaje y análisis crítico de su aplicación en población infantil con discapacidad auditiva. Rev investig Logop. 2018;8(2):147-64. doi.org/10.5209/RLOG.58201
18. Karltorp E, Eklof M, Óstlund M, Asp F, Tideholm B, Lofkvist U. Cochlear implants before 9 months of age led to more natural spoken language development without increased surgical risks. Acta Paediatrica. 2020;109:332-341. doi: 10.1111/apa.14954
19. Singh S, Vashist S, Ariyaratne T. One-year experience with the Cochlear™ Paediatric Implanted Recipient Observational Study (Cochlear P-IROS) in New Delhi, India Journal of Otology. 2015;10:57-65 doi.org/10.1016/j.joto.2015.09.002
20. Czerniejewska-Wolska H, Kałos M, Sekula A, Piszczatowski B, Rutkowska J, Rogowski M, et al. Quality of life and hearing after cochlear implant placement in patients over 60 years of age. Otolaryngol Pol. 2015;69(4):34-39. doi: 10.5604/00306657.1163575
21. Dev A, Adhikari S. Assessment of quality of life outcomes with the glasgow children’s benefit inventory following cochlear implantation in children. J Laryngol Otol. 2019;7:1-5. doi.org/10.1017/S0022215119001555
22. Santos NPD, Couto MIV, Martinho-Carvalho AC. Nijmegen Cochlear Implant Questionnaire (NCIQ): translation, cultural adaptation, and application in adults with cochlear implants. In Codas. 2017;29(6):e20170007-e20170007. doi:10.1590/2317-1782/20172017007
23. Mcrackan T, Bauschard M. Meta-analysis of Quality of Life improvement after Cochlear Implantation and Associations With Speech Recognition Abilities. Laryngoscope. 2018;(128):982-90. Doi:10.1097/AUD.0000000000000684
24. Nordvik O, Laugen P, Bránnström J, Vassbotn F, Aarstad A, Aarstad H. Generic quality of life in persons with hearing loss: a systematic literature Review. BMC Ear Nose Throat Disord. 2018;18:1. Doi:10.1186/s12901-018-0051-6.
25. Sarant J, Harris D, Busby P, Maruff P, Schembri A, Dowell R, Briggs R. The Effect of Cochlear Implants on Cognitive Function in Older Adults: Initial Baseline and 18-Month Follow Up Results for a Prospective International Longitudinal Study. Front Neurosci. 2019;13:789. doi:10.3389/fnins.2019.00789
Published
How to Cite
Issue
Section
License
Copyright (c) 2021 Antonio Simeón Paz-Cordovez, Lidia Charroó-Ruíz, Sandra Bermejo-Guerra, Manuel Enrique Sevila-Salas, Elisa Leyva-Montero

This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License.
Copyright: Camagüey Medical Archive Magazine, offers immediately after being indexed in the SciELO Project; Open access to the full text of the articles under the principle of making available and free the research to promote the exchange of global knowledge and contribute to a greater extension, publication, evaluation and extensive use of the articles that can be used without purpose As long as reference is made to the primary source.
Conflicts of interest: authors must declare in a mandatory manner the presence or not of conflicts of interest in relation to the investigation presented.
(Download Statement of potential conflicts of interest)
The Revista Archivo Médico de Camagüey is under a License Creative Commons Attribution-Noncommercial-No Derivative Works 4.0 International (CC BY 4.0).
This license allows others to distribute, to mix, to adjust and to build from its work, even for commercial purposes, as long as it is recognized the authorship of the original creation. This is the most helpful license offered. Recommended for maximum dissemination and use of licensed materials. The full license can be found at: https://creativecommons.org/licenses/












 22 julio 2025
22 julio 2025