Relationship among location, length of symptoms and reducibility of intussusception in children
Keywords:
invaginación intestinal, reductibilidad, localización de la invaginaciónAbstract
Background: it has been proposed that the location of intussusception in children is directly related to the length of symptoms, and that the more distal the intussusception is, the lower the rate of reduction.
Objective: to determine the relationship of the location of the intussusception with the length of symptoms and the reducibility.
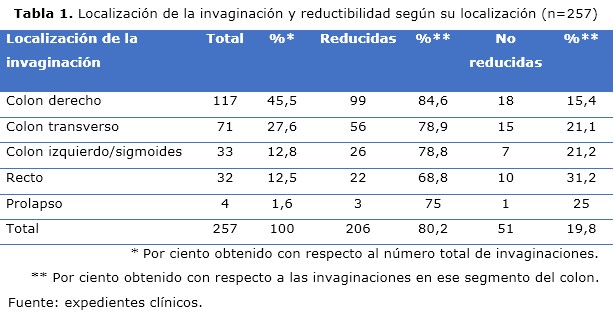
Methods: a descriptive cross-sectional study was carried out in patients between three months and two years of age with intussusception at the Eduardo Agramonte Piña Provincial Pediatric Hospital in Camagüey, from January 2001 to December 2019. The universe of patients consisted of 257 children with intussusception treated by this method, including initial episodes and recurrences.The diagnosis was confirmed by ultrasound. Hydrostatic reduction with saline enemas and ultrasound guidance was attempted in all cases that met the inclusion criteria. The studied variables were: location of intussusception, length of symptoms and reducibility. Statistical decision methods were used in the modeling of the phenomenon under study to determine the statistical dependence / independence of the variables.
Results: the right colon was the most frequent location of the apex of intussusception. The most distal locations (left colon/sigmoid, rectum and prolapsed), although less frequent, it had a high percentage of reducibility. In these locations, reducibility was high both in patients in the first 24 hours of evolution and in those with 25 to 36 hours of onset of symptoms.
Conclusions: direct relationship between location of intussusception and length of symptoms and between location and reducibility was not found.
DeCS: INTUSUSCEPTION; CHILD; INTESTINAL OBSTRUCTION; COLON; SIGN AND SYMPTOMS.
Downloads
References
1. Wright TN, Fallat ME. Intussusception. En: Holcomb GW, Murphy JP, St. Peter S. Holcomb and Ashcraft’s Pediatric Surgery. 7ma ed [Internet]. Philadelphia: Elsevier; 2020 [citado 24 Nov 2020].p. 622-8. Disponible en: https://www.elsevier.com/books/ashcrafts-pediatric-surgery/holcomb/978-0-323-54940-0
2. Marsicovetere P, Ivatury J, White B, Holubar SD. Intestinal Intussusception: Etiology, diagnosis and treatment. Clin Colon Rectal Surg [Internet]. 2017 Feb [citado 24 Nov 2020];30(1):[aprox. 9 p.]. Disponible en: https://www.thieme-connect.com/products/ejournals/pdf/10.1055/s-0036-1593429.pdf
3. Till H, Sorantin E. Intussusception. En: Puri P, Höllwarth ME, editors. Pediatric Surgery. 2da ed [Internet]. Berlin: Springer-Verlag;2019 [citado 24 Nov 2020]. p. 279-86. Disponible en: https://www.springer.com/gp/book/9783540695592
4. Elrouby A, Waheeb S, Ettaby A, Elabany A. Clinical and radiological predictors of the outcome of hydrostatic reduction of primary intussusception in childhood. Alex J Pediatr [Internet]. 2019 [citado 24 Nov 2020]; 32(3): [aprox. 6 p.]. Disponible en: https://www.ajp.eg.net/article.asp?issn=1687-9945;year=2019;volume=32;issue=3;spage=101;epage=106;aulast=Elrouby
5. Reymond RD. The mechanism of intussusception: theorical analysis of the phenomenon. Br J Radiol [Internet]. 1972 Ene [citado 24 Nov 2020];45(529):[aprox. 7 p.]. Disponible en: https://pubmed.ncbi.nlm.nih.gov/5008327/.
6. Pikus HJ, Griffiths AL, Hutson JM. Length of intussusception as a function of mesenteric anatomy. Pediatr Surg Int [Internet]. 1993 [citado 24 Nov 2020];8(2):[aprox. 2 p.]. Disponible en: https://link.springer.com/article/10.1007/BF00184214
7. Stephenson CA, Seibert JJ, Strain JD, Glasier CM, Leithiser RE, Iqbal V. Intussusception: clinical and radiographic factors influencing reducibility. Pediatr Radiol [Internet]. 1989 [citado 24 Nov 2020];20(1-2):[aprox. 3 p.]. Disponible en: https://pubmed.ncbi.nlm.nih.gov/2602017/.
8. He N, Zhang S, Ye X, Zhu X, Zhao Z, Sui X. Risk factors associated with failed sonographically guided saline hydrostatic intussusception reduction in children. J Ultrasound Med [Internet]. 2014 Sep [citado 24 Nov 2020];33(9):[aprox. 6 p.]. Disponible en: https://pubmed.ncbi.nlm.nih.gov/25154951/.
9. Flores Ruiz E, Miranda Novales MG, Villasís Keever MA. El protocolo de investigación VI: cómo elegir la prueba estadística adecuada. Estadística inferencial. Rev Alerg Méx [Internet]. Jul-Sep 2017 [citado 24 Nov 2020];64(3):[aprox. 7 p.]. Disponible en: http://www.scielo.org.mx/pdf/ram/v64n3/2448-9190-ram-64-03-0364.pdf https://doi.org/10.29262/ram.v64i3.304
10. Tellado MG, Liras J, Méndez R, Somoza I, Sánchez A, Maté A, et al. Reducción hidrostática guiada por ecografía para el tratamiento de la invaginación intestinal idiopática. Cir Pediatr [Internet]. Oct 2003 [citado 24 Nov 2020];16(4):[aprox. 3 p.]. Disponible en: https://www.secipe.org/coldata/upload/revista/2003;16.166-8.pdf
11. Ko HS, Schenk JP, Tröger J. Rohrschneider WK. Current radiological management of intussusception in children. Eur Radiol [Internet]. 2007 Sep [citado 24 Nov 2020];17(9):[aprox. 10 p.]. Disponible en: https://pubmed.ncbi.nlm.nih.gov/17308922/.
12. Basu S. Trans-anal protrusion of intussusception (TAPI) revisited: managed successfully in a resource limited hospital setting. Int Surg J [Internet]. 2019 Ene [citado 24 Nov 2020];6(1):[aprox. 3 p.]. Disponible en: https://www.ijsurgery.com/index.php/isj/article/view/3675/2573
13. Mburu E, Akello W, Kimani W, Saula PW, Kuremu RT. Trans-anal protrusion of intussusception. J Pediatr Surg Case Rep [Internet]. 2020 [citado 24 Nov 2020];55 (5):101405. Disponible en: https://www.sciencedirect.com/science/article/pii/S2213576620300385
14. Soria Gondek A, Riaza L, Cuadras D, Tarrado Castellarnau X, Krauel L. Ileocolic intussusception: Predicting the probability of success of ultrasound guided saline enema from clinical and sonographic data. J Pediatr Surg [Internet]. 2018 Abr [citado 24 Nov 2020];53(4):[aprox. 5 p.]. Disponible en: https://pubmed.ncbi.nlm.nih.gov/29150367/.
15. Gfroerer S, Fiegel H, Rolle U. Ultrasound-guided reduction of intussusception: a safe and effective method performed by pediatric surgeons. Pediatr Surg Int [Internet]. 2016 Jul [citado 24 Nov 2020];32(7):[aprox. 3 p.]. Disponible en: https://pubmed.ncbi.nlm.nih.gov/27154198/.
16. Talabi AO, Famurewa OC, Bamigbola KT, Sowande OA, Adolabi BI, Adejuyigbe O. Sonographic guided hydrostatic saline enema reduction of childhood intussusception: a prospective study. BMC Emerg Med [Internet]. 2018 Nov [citado 24 Nov 2020];18(1):46. Disponible en: https://bmcemergmed.biomedcentral.com/articles/10.1186/s12873-018-0196-z
17. Avci V, Agengin K, Bilici S. Ultrasound guided reduction of intussusception with saline and evaluating the factors affecting the success of the procedure. Iran J Pediatr [Internet]. 2018 Feb [citado 24 Nov 2020];28(1):e62442. Disponible en: https://sites.kowsarpub.com/ijp/articles/62442.html
18. Edwards EA, Pigg N, Courtier J, Zapala MA, MacKenzie JD, Phelps AS. Intussusception: past, present and future. Pediatr Radiol [Internet]. 2017 Ago [citado 24 Nov 2020];47(9):[aprox. 7 p]. Disponible en: https://link.springer.com/article/10.1007/s00247-017-3878-x
19. Fike FB, Mortellaro VE, Holcomb GW, St Peter SD. Predictors of failed enema reduction in childhood intussusception. J Pediatr Surg [Internet]. 2012 May [citado 24 Nov 2020];47(5):[aprox. 2 p.]. Disponible en: https://pubmed.ncbi.nlm.nih.gov/22595574/.
DOI: 10.1016/j.jpedsurg.2012.01.047
20. Khirallah MG, Eldesouki NI, Elbatarny AM, Arafa MA. Variables determining the success of ultrasound-guided hydrostatic reduction of intussusception in infants: a tertiary center experience. Ann Pediatr Surg [Internet]. 2017 [citado 24 Nov 2020];13(3):[aprox. 3 p.]. Disponible en: https://www.ajol.info/index.php/aps/article/view/166994/156433
21. Katz M, Phelan E, Carlin JB, Beasley SW. Gas enema for the reduction of intussusception: Relationship between clinical signs and symptoms and outcome. Am J Roentgenol [Internet]. 1993 Feb [citado 24 Nov 2020];160(2):[aprox. 3 p.]. Disponible en: https://pubmed.ncbi.nlm.nih.gov/8424351/.
22. Ong NT, Beasley SW. Progression of intussusception. J Pediatr Surg [Internet]. 1990 Jun [citado 24 Nov 2020];25(6):[aprox. 2 p.]. Disponible en: https://pubmed.ncbi.nlm.nih.gov/2359001/.
23. Bines JE, Ivanoff B. Acute intussusception in infants and children: a global perspective. Immunization, Vaccines and Biologicals [Internet]. Geneva: WHO; 2002 [citado 24 Nov 2020]. 98 p. Disponible en: https://apps.who.int/iris/bitstream/handle/10665/67720/WHO_V-B_02.19_eng.pdf?sequence=1&isAllowed=y
24. Akello VV, Cheung M, Kurigamba G, Semakula D, Healy JM, Grabski D, et al. Pediatric intussusception in Uganda: differences in management andoutcomes with high-income countries. J Pediatr Surg [Internet]. 2020 Mar [citado 24 Nov 2020];55(3):[aprox. 4 p.]. Disponible en: https://www.jpedsurg.org/article/S0022-3468(19)30456-7/fulltext
25. Applegate KE, Sadigh G. Intussusception in infants and children: Diagnostic evidence-based emergency imaging and treatment. En: Kelly A, Cronin P, Puig S, Applegate K, editors. Evidence-Based Emergency Imaging [Internet]. Switzerland: Springer; 2018 [citado 24 Nov 2020]. p. 567-82. Disponible en: https://www.springer.com/gp/book/9783319670645
26. Ramachandran P, Vincent P, Prabhu S, Sridharan S. Rectal prolapse of intussusception - A single institution's experience. Eur J Pediatr Surg [Internet]. 2006 Dic [citado 24 Nov 2020];16(6):[aprox. 2 p.]. Disponible en: https://pubmed.ncbi.nlm.nih.gov/17211791/.
27. Ibrahim IA. Prolapsed ileocolic intussusception. Ann Pediatr Surg [Internet]. 2011 [citado 24 Nov 2020];7(2):[aprox. 3 p.]. Disponible en: https://www.ajol.info/index.php/aps/article/view/95309
28. Mutua I, Ransom J, Kiptoon D. Trans-anal prolapse of ileo-colic intussusception. J Pediatr Surg Case Reports [Internet]. 2018 [citado 24 Nov 2020];38:[aprox. 3 p.]. Disponible en: https://www.clinicalkey.es/#!/content/journal/1-s2.0-S2213576618301519
Published
How to Cite
Issue
Section
License
Copyright (c) 2021 Elizabeth Hernández-Moore, Mauro Castelló-González, Dayamnelis Aguilar-Atanay, Ramón López-Guerrero, Enrique Loret de-Mola-Pino

This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License.
Copyright: Camagüey Medical Archive Magazine, offers immediately after being indexed in the SciELO Project; Open access to the full text of the articles under the principle of making available and free the research to promote the exchange of global knowledge and contribute to a greater extension, publication, evaluation and extensive use of the articles that can be used without purpose As long as reference is made to the primary source.
Conflicts of interest: authors must declare in a mandatory manner the presence or not of conflicts of interest in relation to the investigation presented.
(Download Statement of potential conflicts of interest)
The Revista Archivo Médico de Camagüey is under a License Creative Commons Attribution-Noncommercial-No Derivative Works 4.0 International (CC BY 4.0).
This license allows others to distribute, to mix, to adjust and to build from its work, even for commercial purposes, as long as it is recognized the authorship of the original creation. This is the most helpful license offered. Recommended for maximum dissemination and use of licensed materials. The full license can be found at: https://creativecommons.org/licenses/











 22 julio 2025
22 julio 2025