Results of surgical treatment of patients with lung cancer
Abstract
Background: the incidence of lung cancer in the province of Sancti Spíritus is high and its diagnosis is usually made in advanced stages, for which surgical treatment is not always possible.
Objective: to analyze the main characteristics and results of patients operated on for lung cancer.
Methods: a cross-sectional descriptive observational study was carried out in the General Surgery service of the Camilo Cienfuegos General University Hospital in the Sancti Spiritus province in the period between January 1996 and December 2019. The universe consisted of 83 patients operated with lung cancer who underwent resection accompanied by mediastinal lymph node sampling.
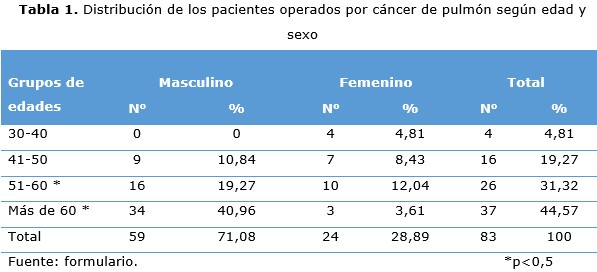
Results: the male sex predominated in the studied group. The most frequent age groups for both sexes were those from 51 to 60 years old and those over 60 years old. Smoking was present in most of the patients. The most frequent tumor location was in the upper lobes and lobectomy was the most performed technique. The pathological stages that predominated were lB and llB, followed by lllA. Squamous cell carcinoma was the predominant histological type. Atelectasis and respiratory infections were the most frequent complications. The deceased were few.
Conclusions: the demographic characteristics of the patients studied correspond to other series of patients with lung cancer. Tumor location in the upper lobes, squamous cell carcinoma, as well as early stages, predominated in the series studied. Lobectomy was the most frequently used surgical technique and among complications, respiratory ones were the most frequent.
DeCS: LUNG NEOPLASMS/surgery; LUNG NEOPLASMS/diagnosis; LUNG NEOPLASMS/complications; PNEUMONECTOMY/methods; CARCINOMA, SQUAMOUS CELL/complications.
Downloads
References
1. Garza Salazar JG de la, Juárez Sánchez P. Antecedentes. En: Garza Salazar JG de la, Juárez Sánchez P, editores. El Cáncer. Ciencia a tu Alcance. México, Nuevo León: Universidad Autónoma de Nuevo León; 2013 p. 17–33.
2. Siegel RL, Miller KD, Jemal A. Cancer statistics, 2020. CA Cancer J Clin [Internet]. 2020 [citado 24 Jul 2018];70(1):7-30. Disponible en: https://pubmed.ncbi.nlm.nih.gov/31912902/.
3. Mao Y, Yang D, He J, Krasna MJ. Epidemiology of Lung Cancer. Surg Oncol Clin N Am [Internet]. Jul 2016 [citado 06 Oct 2020];25(3):439-45. Disponible en: https://cbc.org.br/wp-content/uploads/2016/07/072016SCOe.pdf
4. Choe G, Schipper P. Quality of Lymph Node Assessment and Survival among patients with Non-Small Cell Lung Cancer. JAMA Oncol [Internet]. 2018 Jan [citado 06 Oct 2020];4(1):[aprox. 2 p.]. Disponible en:
https://jamanetwork.com/journals/jamaoncology/fullarticle/2655006
5. MINSAP. Anuario Estadístico de la Salud Cuba 2019. La Habana: Dirección de Registros Médicos y Estadísticas de Salud; 2020 [citado 06 Oct 2020];[aprox. 193 p.]. Disponible en:
https://files.sld.cu/bvscuba/files/2020/05/Anuario-Electr%c3%b3nico-Espa%c3%b1ol-2019-ed-2020.pdf
6. Undurraga PA. Conferencia Dr. Hernán Alessandri R. 2011: Historia del Cáncer Pulmonar: otro monstruo creado por el hombre. Rev Chil Enferm Respir [Internet]. 2012 [citado 06 Oct 2020];28(1):35-50. Disponible en: https://scielo.conicyt.cl/pdf/rcher/v28n1/art06.pdf
7. Putnam JB. Pulmón, Pared Torácica, Pleura y Mediastino. En: Townsend CM, Beauchamp RD, Evers BM, Mattox KL, editors. Tratado de Cirugía de Sabiston y Cols. 19ª ed. Barcelona: Elselvier W.B. Saunders; 2019. p 1565–1610.
8. Quirós Hernández JL, González Ferrer V, Cárdenas García R. Caracterización epidemiológica de pacientes con cáncer de pulmón. Hospital Celestino Hernández Robau, Villa Clara. Medicentro Electrón [Internet]. 2014 [citado 06 Oct 2020];18(2):[aprox. 7 p.]. Disponible en:
http://www.medicentro.sld.cu/index.php/medicentro/article/view/1706/1358
9. Graña Aramburú A. Breve evolución histórica del cáncer. Carcinus [Internet]. 2015 [citado 03 Ene 2019];5(1):[aprox. 6 p.]. Disponible en:
http://www.imbiomed.com.mx/1/1/descarga.php?archivo=Pe-On1501-06r.pdf
10. MINSAP. Informe Anual Estadístico de Salud 2016. Incidencia de cáncer del pulmón en la provincia de Camagüey. Camagüey: Dirección Provincial de Salud Pública, Departamento Provincial de Estadísticas y Registros Médicos; 2016.
11. MINSAP. Informe Anual Estadístico de Salud 2019. Incidencia de cáncer del pulmón en la provincia de Sancti Spiritus. Sancti Spiritus: Dirección Provincial de Salud Pública, Departamento Provincial de Estadísticas y Registros Médicos; 2019.
12. Wakelee HA, Gomez SL, Chang ET. Sex differences in lung-cancer susceptibility: a smoke screen? Lancet Oncol. 2008 Jul;9(7):649-56.
13. Barrionuevo CC, Dueñas Hancco D. Clasificación actual del carcinoma de pulmón. Consideraciones histológicas, inmunofenotípicas, moleculares y clínicas. Horiz Med [Internet]. Oct 2019 [citado 06 Oct 2020];19(4):74-83. Disponible en: http://www.scielo.org.pe/scielo.php?script=sci_arttext&pid=S1727558X2019000400011&lng=es
14. Pérez Guerra LE, Rodríguez Flores O, Morales Morales Y, Amores Ramos A, Jaime Valdés LM, Pérez Rodríguez A. Cáncer de Pulmón: Aspectos clínicos y diagnósticos en pacientes afectados del Policlínico Marta Abreu. Estudio de cinco años. Acta Médica Centro [Internet]. 2017 [citado 06 Oct 2020];11(3). Disponible en: http://www.revactamedicacentro.sld.cu/index.php/amc/article/view/833/1051
15. Rami-Porta R. The IASLC Lung Cancer Staging Project. Proposals for the Revisions of the T Descriptors in the Forthcoming Eighth Edition of the TNM Classification for Lung Cancer. J Thorac Oncol; 2015;10:990–1003.
16. Sepsas E, Vachlas K, Gaitanakis S, Toufektzian L, Kainis E, Gkiozos I. Recurrence in patients that underwent surgery for lung cancer. Pneumon [Internet]. 2017 [citado 06 Oct 2020];30(3):133-40. Disponible en:
17. Hom L, Lima Araujo L, Nana-Simkam, Otterson G, Williams, Carbone DP. Molecular Biology of Lung Cancer. In: DeVita`s, editor. Cancer: Principles & Practice of Oncology. 10th ed. Philadelphia: Lippincott Williams&Wilkins; 2015 p. 482–93.
18. Mamolar Herrera N. Supervivencia a largo plazo de pacientes operados de cáncer de pulmón. Del análisis de los datos a un diseño de seguimiento útil [tesis]. España: Universidad de Valladolid, Facultad de Medicina; 2017 [citado 06 Oct 2020]. Disponible en: http://uvadoc.uva.es/handle/10324/24093
19. Barbosa IR, Bernal Pérez MM, Costa CC, Jerez-Roig J, de Souza DLB. Supervivencia del cáncer de pulmón en pacientes tratados en un hospital de referencia en Zaragoza. Semergen [Internet]. 2016 [citado 06 Oct 2020];42(6):380-7. Disponible en:
https://www.sciencedirect.com/science/article/abs/pii/S113835931500266X
20. Riquet M, Pricopi C, Arame A, Le Pimpec Barthes F. From anatomy to lung cancer: questioning lobe-specific mediastinal lymphadenectomy reliability. J Thorac Dis. 2016;8(9):2387-90.
21. Deng Y, Wang J, Mu J, Wang Z, Wang G. Complete Uniportal Thoracoscopic Anatomic Lung Resection With Systematic Mediastinal Lymphadenectomy for Non-Small Cell Lung Cancer: Personal Experience of 326 Cases. Surg Laparosc Endosc Percutan Tech [Internet]. 2020 [citado 06 Oct 2020];30(2):173-9. Disponible en:
https://journals.lww.com/surgical-laparoscopy/Fulltext/2020/04000/Complete
_Uniportal_Thoracoscopic_Anatomic_Lung.14.aspx
22. Felipe Font E, Cedrés Pérez S. Tratamiento. Estadios I y II y tratamiento adyuvante. En: Cortés-Funes H, Colomer Boch R, editores. Tratado de oncología. Barcelona: Publicaciones Permanyer; 2009.p. 631-6.
23. Wang W, Chen D, Xi K, Chen Y, Zhang X, Wen Y, et al. Impact of Different Types of Lymphadenectomy Combined With Different Extents of Tumor Resection on Survival Outcomes of Stage I Non-small-cell Lung Cancer: A Large-Cohort Real-World Study. Front Oncol [Internet]. 2019 Jul 24 [citado 06 Oct 2020];9:642. Disponible en: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6668052/.
24. Wang Y, Darling GE. Complete mediastinal lymph node dissection versus systematic lymph node sampling in surgical treatment of non-small cell lung cancer: do we have the answer? J Thorac Dis [Internet]. 2017 [citado 06 Oct 2020];9(11): 4169-70. Disponible en: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5721010/.
25. Wo Y, Zhao Y, Qiu T, Li S, Wang Y, Lu T, et al. Impact of visceral pleural invasion on the association of extent of lymphadenectomy and survival in stage I non-small cell lung cancer. Cancer Med [Internet]. Feb 2019 [citado 06 Oct 2020];8(2):669-78. Disponible en: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6382711/.
26. Meng D, Zhou Z, Wang Y, Wang L, Lv W, Hu J. Lymphadenectomy for clinical early-stage non-small-cell lung cancer: a systematic review and meta-analysis. Eur J Cardiothorac Surg [Internet]. 2016 [citado 06 Oct 2020];50(4):597-604. Disponible en: https://academic.oup.com/ejcts/article/50/4/597/2197354
27. Hayashi T, Sakakura N, Ishimura D, Kozawa E, Yoshida M, Sakao Y, et al. Surgical complication and postoperative pulmonary function in patients undergoing tumor surgery with thoracic wall resection. Oncol Lett [Internet]. 2019 [citado 06 Oct 2020];17(3):3446-3456. Disponible en: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6396184/.
28. Martos Benítez FD, Echevarría Víctores A, Echevarría Soulary JC, Gutiérrez Noyola A, Candales Arafet LA, Pupo San Juan YY. Repercusión de las complicaciones mayores posoperatorias en pacientes operados de tórax. Rev Cubana Cir [Internet]. Dic 2014 [citado 06 Oct 2020];53(4):366-377. Disponible en: http://scielo.sld.cu/scielo.php?script=sci_arttext&pid=S0034-74932014000400005&lng=es
Published
How to Cite
Issue
Section
License
Copyright (c) 2021 Orlando Silvio Rodríguez-Martínez, Miguel Emilio García-Rodríguez, Miguel Alexánder Concepción-López, Jorge Héctor Rojas-Sánchez, Sandra Moreno-Perera

This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License.
Copyright: Camagüey Medical Archive Magazine, offers immediately after being indexed in the SciELO Project; Open access to the full text of the articles under the principle of making available and free the research to promote the exchange of global knowledge and contribute to a greater extension, publication, evaluation and extensive use of the articles that can be used without purpose As long as reference is made to the primary source.
Conflicts of interest: authors must declare in a mandatory manner the presence or not of conflicts of interest in relation to the investigation presented.
(Download Statement of potential conflicts of interest)
The Revista Archivo Médico de Camagüey is under a License Creative Commons Attribution-Noncommercial-No Derivative Works 4.0 International (CC BY 4.0).
This license allows others to distribute, to mix, to adjust and to build from its work, even for commercial purposes, as long as it is recognized the authorship of the original creation. This is the most helpful license offered. Recommended for maximum dissemination and use of licensed materials. The full license can be found at: https://creativecommons.org/licenses/












 22 julio 2025
22 julio 2025