Evaluation of transcervical lymphadenectomy in the diagnostic system of lung cancer
Abstract
Background: the lymph node study of the mediastinum in patients with lung cancer is of vital importance, as it allows the therapeutic strategy to be outlined.
Objective: to evaluate the transcervical lymphadenectomy technique as part of the diagnostic system in lung cancer.
Methods: a prospective longitudinal analytical investigation was carried out in patients in whom transcervical lymphadenectomy was used as part of the diagnostic system for lung cancer at the Hospital Universitario Manuel Ascunce Domenech, in the province of Camagüey. The universe was made up of 346 patients and the sample, of a simple random probability type, consisted of 65 patients.
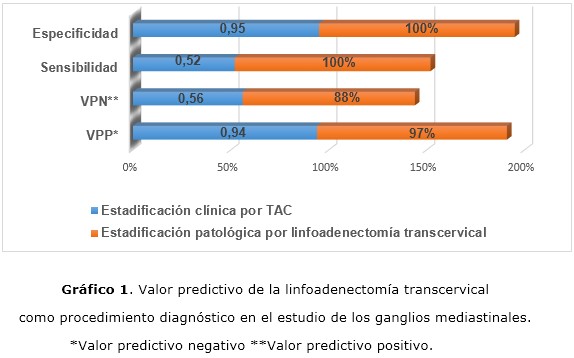
Results: male patients over 60 years prevailed. The most frequent histological type was adenocarcinoma and the upper lobes were the most affected. A total of 205 nodes were removed and the majority were positive, negativity, in histology, predominated in nodes less than 1 cm diagnosed in the tomographic study. There was migration of stages in the clinical pathological correlation, as well as the sensitivity and specificity were 100% in the studied sample. Complications were rare.
Conclusions: transcervical lymphadenectomy constitutes a diagnostic tool in patients with lung cancer and mediastinal lymph node involvement.
DeCS: LUNG NEOPLASMS/surgery; LUNG NEOPLASMS/complications; LUNG NEOPLASMS/diagnostic imaging; LYMPH NODE EXCISION/methods; LONGITUDINAL STUDIES.
Downloads
References
1. Siegel RL, Miller KD, Jemal A. Cancer statistics, 2018. CA Cancer J Clin [Internet]. 2018 Jan [citado 24 Jul 2018];68(1):[aprox. 10 p.]. Disponible en: https://onlinelibrary.wiley.com/doi/full/10.3322/caac.21442
2. Bray F, Ferlay J, Soerjomataram I, Siegel RL, Torre LA, Jemal A. Global cancer statistics 2018: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J Clin [Internet]. 2018 Nov [citado 12 Dic 2018];68(6):[aprox. 7 p.]. Disponible en:
https://onlinelibrary.wiley.com/doi/full/10.3322/caac.21492
3. Radovic M, Kanesvaran R, Rittmeyer A, Fruh M, Minervini F, Glatzer M, et al. Multidisciplinary treatment of lung cancer in older patients: A review. J Geriatr Oncol. 2019;10(3):405-10.
4. Edwards JG, Chansky K, Van Schil P, Nicholson AG, Boubia S, Brambilla E, et al. The IASLC Lung Cancer Staging Project: Analysis of Resection Margin Status and Proposals for Residual Tumor Descriptors for Non-Small Cell Lung Cancer. J Thorac Oncol. 2020;15(3):344-59.
5. Fernandez FG, Kosinski AS, Furnary AP, Onaitis M, Kim S, Habib RH, et al. Differential effects of operative complications on survival after surgery for primary lung cancer. J Thorac Cardiovasc Surg [Internet]. 2018 Mar [citado 12 Dic 2018];155(3):[aprox. 10 p.]. Disponible en: https://www.jtcvs.org/article/S0022-5223(17)32503-5/pdf
6. Huang M, Manuballa S, Demmy T, Yendamuri S. Transcervical Extended Mediastinal Lymphadenectomy-Indications and Technique. Indian J Surg Oncol [Internet]. 2013 Jun [citado 24 Jul 2018];4(2):[aprox. 3 p.]. Disponible en: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3693144/.
7. Pérez Alonso D, Hernández Escobar F, López Rivero L. Incisional metastasis from lung cancer after transcervical extended mediastinal lymphadenectomy. Arch Bronconeumol. 2016;52(5):276-7.
8. Yendamuri S, Battoo A, Dy G, Chen H, Gomez J, Singh AK, et al. Transcervical Extended Mediastinal Lymphadenectomy: Experience From a North American Cancer Center. Ann Thorac Surg. 2017;104(5):1644-9.
9. Kuzdzal J, Zielinski M, Papla B, Urbanik A, Wojciechowski W, Narski M, et al. The transcervical extended mediastinal lymphadenectomy versus cervical mediastinoscopy in non-small cell lung cancer staging. Eur J Cardiothorac Surg. 2007;31(1):88-94.
10. Zieliński M. Transcervical extended mediastinal lymphadenectomy. Thorac Surg Clin. 2010;20(2):215-223.
11. Jawad H, Sirajuddin A, Chung JH. Review of the International Association for the Study of Lung Cancer Lymph Node Classification System Localization of Lymph Node Stations on CT Imaging. Clin Chest Med [Internet]. 2013 Sep [citado 24 Jul 2018];34(3):[aprox. 7 p.]. Disponible en: https://www.clinicalkey.es/service/content/pdf/watermarked/1-s2.0-S0272523113000579.pdf?locale=es_ES
12. Benn BS, Parikh M, Tsau PH, Seeley E, Krishna G. Using a Dedicated Interventional Pulmonology Practice Decreases Wait Time Before Treatment Initiation for New Lung Cancer Diagnoses. Lung [Internet]. 2019 Feb 19 [citado 20 Feb 2019]. Disponible en:
https://link.springer.com/content/pdf/10.1007%2Fs00408-019-00207-6.pdf
13. Li L, Liu D, Zhang L, Zhou P, Song J, Cheng Y, et al. Clinicopathological Features, Diagnoses and Treatments of 6 458 Lung Cancer Patients. Sichuan Da Xue Xue Bao Yi Xue Ban. 2017 May;48(3):352-8.
14. Jawad H, Sirajuddin A, Chung JH. Review of the International Association for the Study of Lung Cancer Lymph Node Classification System Localization of Lymph Node Stations on CT Imaging. Clin Chest Med [Internet]. 2013 Sep [citado 24 Jul 2018];34(3):[aprox. 7 p.]. Disponible en: https://www.clinicalkey.es/service/content/pdf/watermarked/1-s2.0-S0272523113000579.pdf?locale=es_ES
15. Akalin A, Ergin A, Remiszewski S, Mu X, Raz D, Diem M. Resolving Interobserver Discrepancies in Lung Cancer Diagnoses by Spectral Histopathology. Arch Pathol Lab Med [Internet]. 2019 Feb [citado 13 Feb 2019];143(2):[aprox. 10 p.]. Disponible en:
https://www.archivesofpathology.org/doi/pdf/10.5858/arpa.2017-0476-SA
16. Göke A, Göke R, Ofner A, Herbst A, Lankat-Buttgereit B. The FGFR Inhibitor NVP-BGJ398 Induces NSCLC Cell Death by Activating Caspase-dependent Pathways as well as Caspase-independent Apoptosis. Anticancer Res [Internet]. 2015 Nov [citado 24 Jul 2018];35(11):[aprox. 9 p.]. Disponible en:
http://ar.iiarjournals.org/content/35/11/5873.long
17. Deslauries J. Mediastinal lymph nodes: Ignore? Sample? Dissect? The role of mediastinal node dissection in the surgical management of primary lung cancer. Gen Thorac Cardiovasc Surg [Internet]. 2012 Nov [citado 24 Jul 2018];60(11):[aprox. 10 p.]. Disponible en: https://link.springer.com/article/10.1007%2Fs11748-012-0086-3
18. De Leyn P, Dooms C, Kuzdzal J, Lardinois D, Passlick B, Rami-Porta R, et al. Revised ESTS guidelines for preoperative mediastinal lymph node staging for non-small-cell lung cancer. Eur J Cardiothorac Surg [Internet]. 2014 May [citado 24 Jul 2018];45(5):[aprox. 11 p.]. Disponible en:
http://www.ests.org/_userfiles/pages/files/Revised%20ESTS%20Guidelines(1).pdf
19. Yang H, Yao F, Zhao Y, Zhao H. Clinical outcomes of surgery after induction treatment in patients with pathologically proven N2-positive stage III non-small cell lung cancer. J Thorac Dis [Interne]. 2015 Sep [citado 24 Jul 2018];7(9):[aprox. 7 p.]. Disponible en: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4598515/.
20. Eberhardt W, Pottgen C, Gauler T, Friedel G, Veit S, Heinrich V, et al. Phase III Study of Surgery Versus Definitive Concurrent Chemoradiotherapy Boost in Patients With Resectable Stage IIIA(N2) and Selected IIIB Non-Small-Cell Lung Cancer After Induction Chemotherapy and Concurrent Chemoradiotherapy (ESPATUE). J Clin Oncol [Internet]. 2015 Dec 10 [citado 24 Jul 2018];33(35):[aprox. 11 p.]. Disponible en:
21. Dong S, Du J, Li W, Zhang S, Zhong X, Zhang L. Systematic mediastinal lymphadenectomy or mediastinal lymph node sampling in patients with pathological stage I NSCLC: a meta-analysis. World J Surg [Internet]. 2015 Feb [citado 24 Jul 2018];39(2):[aprox. 13 p.]. Disponible en: https://link.springer.com/article/10.1007%2Fs00268-014-2804-8
22. Wang Y, Wu N, Chen J, Lv C, Yan S, Li S, et al. Is radical mediastinal lymphadenectomy necessary for elderly patients with clinical N-negative non-small-cell lung cancer? A single center matched-pair study. J Surg Res [Internet]. 2015 Jan [citado 24 Jul 2018];193(1):[aprox. 13 p.]. Disponible en: https://www.clinicalkey.es/service/content/pdf/watermarked/1-s2.0-S0022480414007859.pdf?locale=es_ES
23. Cheng AW, Shaul DB, Sydorak RM. Success ful thoracoscopic resection of large symptomatic mediastinal lymphatic malformations: Report of 3 cases. J Thorac Cardiovasc Surg [Internet]. 2015 Oct [citado 24 Jul 2018];150(4):[aprox. 9 p.]. Disponible en: https://www.clinicalkey.es/service/content/pdf/watermarked/1-s2.0-S0022522315012301.pdf?locale=es_ES
24. Zielinski M, Szlubowski A, Kolodziej M, Orzechowski S, Laczynska E, Pankowski J, et al. Comparison of endobronchial ultrasound and/or endoesophageal ultrasound with transcervical extended mediastinal lymphadenectomy for staging and restaging of non-small-cell lung cancer. J Thorac Oncol [Internet]. 2013 May [citado 24 Jul 2018];8(5):[aprox. 11 p.]. Disponible en: https://www.jto.org/article/S1556-0864(15)32822-7/fulltext
25. Honguero Martínez AF, García Jiménez MD, García Vicente A, López-Torres Hidalgo J, Colon MJ, van Gómez López O, et al. Ratio between maximum standardized uptake value of N1 lymph nodes and tumor predicts N2 disease in patients with non-small cell lung cancer in 18F-FDG PET-CT scan. Rev Esp Med Nucl Imagen Mol [Internet]. 2016 May-Jun [citado 24 Jul 2018];35(3):[aprox. 9 p.]. Disponible en: https://www.clinicalkey.es/service/content/pdf/watermarked/1-s2.0-S2253654X1500116X.pdf?locale=es_ES
26. López Encuentra A, Gómez de la Cámara A, Varela de Ugarte N, Mañes N, Llobregat N, Grupo Cooperativo de Carcinoma Broncogénico de la Sociedad Española de Neumología y de Cirugía Torácica (GCCB-S). El fenómeno “Will-Rogers”. Migración de estadios en carcinoma broncogénico, tras aplicar criterios de certeza clasificatoria. Arch Bronconeumol. 2002;38(4):166-71.
27. Cuesta MA, van der Peet DL, Gisbertz SS, Straatman J. Mediastinal lymphadenectomy for esophageal cancer: Differences between two countries, Japan and the Netherlands. Ann Gastroenterol Surg [Internet]. 2018 May 1 [citado 24 Jul 2018];2(3):[aprox. 15 p.]. Disponible en: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5980465/.
28. Fabre E, Rivera C, Mordant P, Gibault L, Dujon A, Foucault C, et al. Evolution of induction chemotherapy for non-small cell lung cancer over the last 30 years: A surgical appraisal. Thoracic Cancer [Internet]. 2015 Nov [citado 24 Jul 2018];6(6):[aprox. 14 p.]. Disponible en: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4632925/.
Published
How to Cite
Issue
Section
License
Copyright (c) 2020 Miguel Emilio García-Rodríguez, Kevys Socarras-Montalvan, Miguel Javier García-Basulto, Arian Benavidez-Márquez, Raúl Koelig-Padrón

This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License.
Copyright: Camagüey Medical Archive Magazine, offers immediately after being indexed in the SciELO Project; Open access to the full text of the articles under the principle of making available and free the research to promote the exchange of global knowledge and contribute to a greater extension, publication, evaluation and extensive use of the articles that can be used without purpose As long as reference is made to the primary source.
Conflicts of interest: authors must declare in a mandatory manner the presence or not of conflicts of interest in relation to the investigation presented.
(Download Statement of potential conflicts of interest)
The Revista Archivo Médico de Camagüey is under a License Creative Commons Attribution-Noncommercial-No Derivative Works 4.0 International (CC BY 4.0).
This license allows others to distribute, to mix, to adjust and to build from its work, even for commercial purposes, as long as it is recognized the authorship of the original creation. This is the most helpful license offered. Recommended for maximum dissemination and use of licensed materials. The full license can be found at: https://creativecommons.org/licenses/












 22 julio 2025
22 julio 2025