Prevalence and variables associated with alcohol and tobacco consumption in burned patients
Abstract
Background: current studies have showed that there is a high prevalence of alcohol and tobacco use in burned patients. In Cuba, published research on this topic is scarce.
Objective: to determine the prevalence and associated variables of alcohol and tobacco consumption of burned patients admitted to the Vladimir Ilich Lenin General Teaching Hospital.
Methods: a quantitative cross-sectional descriptive study was carried out. The universe consisted of 73 burned patients admitted to the Burn & Reconstructive Surgery service of the Vladimir Ilich Lenin Teaching Hospital, from January 2018 to December 2019. 62 patients were selected by probabilistic sampling. Semi-structured interviews, observation and documentary review were used for the evaluation. Socio-demographic variables, burning production mode and cause, alcohol and tobacco consumption, state of intoxication on admission and mental disorder during hospitalization were considered as variables. The results were processed with the statistical packages EPIDAT 3.1 and MedCalc.
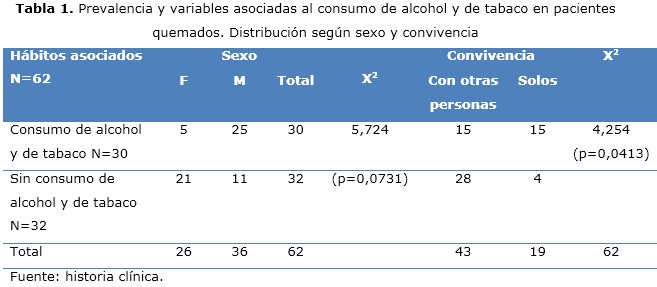
Results: the estimate of the prevalence of alcohol and tobacco use, in general, was relatively high. Male sex, white skin color, rural origin, single marital status with children, accidental burning and the direct fire cause predominated. Most of them had alcohol withdrawal symptoms. Significant associations were obtained between alcohol and tobacco use, in general, with the variables sex, marital status, living with other people, mode of burn production, causal agent and mental disorder.
Conclusions: the prevalence rate of alcohol and tobacco use, in general, was relatively high. An association was found between alcohol and tobacco consumption and the variables sex, marital status, living with other people, mode of burn production, causal agent and mental disorder.
DeCS: ALCOHOLISM/epidemiology; TOBACCO USE DISORDER/epidemiology; BUIRNS/ psychology; BURNS/prevention&control; EPIDEMIOLOGY, DESCRIPTIVE.
Downloads
References
1. WHO. A WHO plan for Burn Prevention and Care [Internet]. Geneva: WHO; 2008 [citado 14 Mar 2020]:[aprox. 32 p.]. Disponible en: https://apps.who.int/iris/bitstream/handle/10665/97852/9789241596299_eng.pdf?sequence=1
2. Ministerio de Salud Pública. Dirección de Registros Médicos y Estadísticas de Salud. Anuario Estadístico de Salud 2018 [Internet]. La Habana: Minsap; 2019 [citado 14 Mar 2020]. Disponible en: http://files.sld.cu/bvscuba/files/2019/04/Anuario-Electrónico-Español-2018-ed-2019.pdf
3. Vera I, Ferrando E, Vidal I, Gómez-Olmeda D, González JC. Burns and Mental Disorder. Rev Psiquiatr Salud Ment (Barc.) [Internet]. 2010 [citado 14 Mar 2020];3(1):19-22. Disponible en: https://www.elsevier.es/en-revista-revista-psiquiatria-salud-mental-486-resumen-burns-mental-disorder-S2173505010700042
4. Gallach E, Pérez MD, Vivó C. Perfil psicológico del paciente gran quemado: prevalencia psicopatológica y variables asociadas. Cir Plást Iberolatinoam [Internet]. 2015 [citado 14 Mar 2019];41(4):436-427. Disponible en: http://scielo.isciii.es/scielo.php?script=sci_arttext&pid=S0376-78922015000400010
5. Steenkamp WC, Botha NJ, Van der Merwe AE. The prevalence of alcohol dependence in burned adult patients. Burns [Internet]. 1994 [citado 14 Mar 2020];20(6):522–5. Disponible en: https://www.ncbi.nlm.nih.gov/pubmed/7880417
6. Rodríguez Vargas M, Rodríguez Ricardo A, Marrero Pérez Y, Durán Cordoves L, Angulo Zaragoza A, Díaz Rojas P. Alteraciones psicológicas en pacientes quemados durante su estadía hospitalaria. CCM [Internet]. 2019 [citado 14 Mar 2020];23(4):[aprox. 2 p.]. Disponible en: http://revcocmed.sld.cu/index.php/cocmed/article/view/3356/1467
7. Palmu R, Partonen T, Suominen K, Vuola J, Isometsä E. Alcohol use and smoking in burn patients at the Helsinki Burn Center. Burns [Internet]. 2018 [citado 14 Mar 2020];44(1):158-167. Disponible en: https://linkinghub.elsevier.com/retrieve/pii/S0305-4179(17)30337-6
8. Klifto KM, Shetty PN, Slavin BR, Gurno CF, Seal SM, Asif M, et al. Impact of nicotine/smoking, alcohol, and illicit substance use on outcomes and complications of burn patients requiring hospital admission: systematic review and meta-analysis. Burns. En prensa; 2019.
9. Grant GG, Wolfe AE, Thorpe CR, Gibran NS, Carrougher GJ, Wiechman SA, et al. Exploring the Burn Model System National Database: Burn injuries, substance misuse, and the CAGE questionnaire. Burns [Internet]. 2020 [citado 14 Mar 2020];46(3):745-747. Disponible en: https://www.clinicalkey.es/#!/content/playContent/1-s2.0-S0305417919308812?returnurl=https:%2F%2Flinkinghub.elsevier.com%2Fretrieve%2Fpii%2FS0305417919308812%3Fshowall%3Dtrue&referrer=https:%2F%2Fwww.ncbi.nlm.nih.gov%2F
10. Chen MM, Carter CR, Curtis BJ, O’Halloran EB, Gamelli RL, Kovacs EJ. Alcohol modulation of the post burn hepatic response. J Burn Care Res [Internet]. 2017 [citado 14 Mar 2020];38(1):e144-57. Disponible en: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4757520/.
11. Rehou S, Mason S, MacDonald J, Pinto R, Jeschke MG. The influence of substance misuse on clinical outcomes following burn. Burns [Internet]. 2017 [citado 14 Mar 2020];43:1493-8. Disponible en: https://www.ncbi.nlm.nih.gov/pubmed/28506508
12. Hodgman EI, Subramanian M, Wolf SE, Arnoldo BD, Phelan HA, Cripps MW, et al. The effect of illicit drug use on outcomes following burn injury. J Burn Care Res [Internet]. 2017 [citado 14 Mar 2020];1:e89-94. Disponible en: https://www.ncbi.nlm.nih.gov/pubmed/28009698
13. Carlos WG, Baker MS, McPherson KA, Bosslet GT, Sood R, Torke AM. Smoking-related home oxygen burn injuries: continued cause for alarm. Respiration [Internet]. 2016 [citado 14 Mar 2020];2:151-5. Disponible en: https://www.ncbi.nlm.nih.gov/pubmed/26812246
14. Afshar M, Netzer G, Mosier MJ, Cooper RS, Adams W, Burnham EL, et al. The Contributing risk of tobacco use for ARDS development in burn-injured adults with inhalation injury. Respir Care [Internet]. 2017 [citado 14 Mar 2020];11:1456-65. Disponible en: https://www.ncbi.nlm.nih.gov/pubmed/28900039
15. Chun LF, Moazed F, Calfee CS, Matthay MA, Gotts JE. Pulmonary toxicity of e-cigarettes. Am J Physiol Lung Cell Mol Physiol [Internet]. 2017 [citado 14 Mar 2020];2:L193-206. Disponible en: https://www.ncbi.nlm.nih.gov/pubmed/28522559
16. Toppi J, Cleland H, Gabbe B. Severe burns in Australian and New Zealand adults: Epidemiology and burn centre care. Burns [Internet]. 2019 [citado 14 Mar 2020];45:1456-1461. Disponible en: https://www.ncbi.nlm.nih.gov/pubmed/31053412
17. Mushin OP, Esquenazi MD, Ayazi S, Craig C, Bell DE. Self-inflicted burn injuries: Etiologies, risk factors and impact on institutional resources. Burns [Internet]. 2019 [citado 14 Mar 2020];45:213-219. Disponible en: https://www.ncbi.nlm.nih.gov/pubmed/30467036
18. Adams C, Locke C, Warner J. Mental health liaison in a regional burns unit-Past, present and future. Burns [Internet]. 2019 [citado 14 Mar 2020];45:1375-1378. Disponible en: https://www.ncbi.nlm.nih.gov/pubmed/31060761
19. Davis CS, Esposito TJ, Palladino AG, Rychlik K, Schermer CR, GamelliR L, Kovacs EJ. Implications of alcohol intoxication at the time of burn and smoke inhalation injury: an epidemiologic and clinical analysis. J Burn Care Res [Internet]. 2013 [citado 14 Mar 2020];34(1):120–126. Disponible en: https://www.ncbi.nlm.nih.gov/pubmed/23079566
20. Poznyak V, Rekve D. Global status report on alcohol and health 2018: Executive summary [Internet]. Geneva: World Health Organization; 2018 [citado 14 Mar 2020]. Disponible en: https://iris.paho.org/bitstream/handle/10665.2/51352/OPSNMH19012_spa.pdf?sequence=1&isAllowed=y
Published
How to Cite
Issue
Section
License
Copyright (c) 2020 Malvin Rodríguez-Vargas

This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License.
Copyright: Camagüey Medical Archive Magazine, offers immediately after being indexed in the SciELO Project; Open access to the full text of the articles under the principle of making available and free the research to promote the exchange of global knowledge and contribute to a greater extension, publication, evaluation and extensive use of the articles that can be used without purpose As long as reference is made to the primary source.
Conflicts of interest: authors must declare in a mandatory manner the presence or not of conflicts of interest in relation to the investigation presented.
(Download Statement of potential conflicts of interest)
The Revista Archivo Médico de Camagüey is under a License Creative Commons Attribution-Noncommercial-No Derivative Works 4.0 International (CC BY 4.0).
This license allows others to distribute, to mix, to adjust and to build from its work, even for commercial purposes, as long as it is recognized the authorship of the original creation. This is the most helpful license offered. Recommended for maximum dissemination and use of licensed materials. The full license can be found at: https://creativecommons.org/licenses/












 22 julio 2025
22 julio 2025