Late tracheostomy and tracheal stenosis in operated post-COVID-19 patients
Abstract
Introduction: COVID-19 is a disease under study. Research is being carried out, with conflicting results. In Peru, studies in this regard are scarce, and it is advisable to focus efforts.
Objective: To characterize post-COVID-19 patients operated on for tracheal stenosis in the Head and Neck Surgery Service of the Alberto Sabogal National Hospital.
Methods: The study was quantitative, with a non-experimental, descriptive, correlational and retrospective design. The electronic medical records of patients who underwent surgery for tracheal stenosis and history of intubation due to COVID-19, during 2020 and 2021, were searched. 74 were found, of which 69 met the inclusion and exclusion criteria. The data obtained was recorded in a Form. Results were processed with SPSS. Absolute and relative frequencies, average, minimum and maximum values and prevalence rate were obtained. Results were represented in statistical tables.
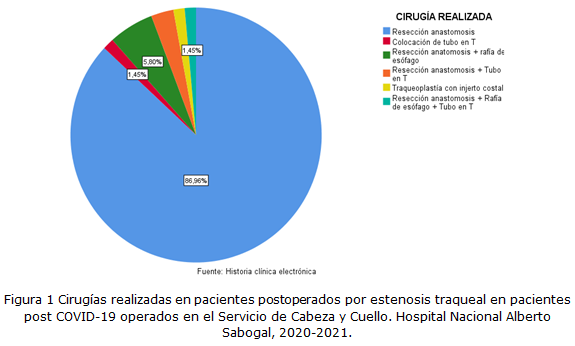
Results: 30.4 % had a history of tracheostomy, 100 % corresponding to late tracheostomy. The average number of days of oral-tracheal intubation was 25 (7-60 days). The location of the stenosis was cervical in 86 %. It was observed that up to 7 % had associated trachea-esophageal fistula. The average number of compromised rings was 5 (3-8). The average percentage of stenosis was 85 % (40-100 %). In relation to the Cotton and Myer classification: 4 % corresponded to grade I, 11 % to grade II, 76 % to grade III and 9 % to grade IV.
Conclusions: The rate of prior tracheostomy is low in patients operated on for tracheal stenosis, all of which corresponds to late tracheostomy. The average number of days of oral-tracheal intubation was 25. The most frequent location was cervical. The average number of involved rings was 5. The average percentage of stenosis was 85 %. Regarding the Cotton and Myer classification: the majority corresponded to grade III. Finally, the most frequent surgery performed was resection and tracheal anastomosis.
DeCS: TRACHEAL STENOSIS/surgery; TRACHEOSTOMY; COVID-19; PATIENTS; PREVALENCE.
Downloads
References
1. Gervasio CF, Averono G, Robiolio L, Bertoletti M, Colageo U, De Col L, et al. Tracheal stenosis after tracheostomy for mechanical ventilation in COVID-19 pneumonia - A report of 2 cases from Northern Italy. American Journal of Case Reports [Internet]. 2020 [citado 26 May 2024]; 21. Disponible en: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7447296/
2. Chao TN, Harbison SP, Braslow BM, Hutchinson CT, Rajasekaran K, Go BC, et al. Outcomes after tracheostomy in COVID-19 patients. Annals of Surgery [Internet]. 2020 [citado 26 May 2024]; 272(3):181–e186. Disponible en:
https://pubmed.ncbi.nlm.nih.gov/32541213/
3. Mattioli F, Fermi M, Ghirelli M, Molteni G, Sgarbi N, Bertellini E, et al. Tracheostomy in the COVID-19 pandemic. Eur Arch Otorhinolaryngol [Internet]. 2020 [citado 26 May 2024];277(7):2133-2135. Disponible en:
https://pubmed.ncbi.nlm.nih.gov/32322959/
4. Piazza C, Filauro M, Dikkers FG, Nouraei SAR, Sandu K, Sittel C, et al. Long-term intubation and high rate of tracheostomy in COVID-19 patients might determine an unprecedented increase of airway stenoses: a call to action from the European Laryngological Society. Eur Arch Otorhinolaryngol [Internet]. 2021 [citado 26 May 2024]; 278(1):1-7. Disponible en:
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7275663/
5. Yang X, Yu Y, Xu J, Shu H, Xia J, Liu H, et al. Clinical course and outcomes of critically ill patients with SARS-CoV-2 pneumonia in Wuhan, China: a single-centered, retrospective, observational study. Lancet Respir Med [Internet]. 2020 [citado 26 May 2024]; 8(5):475-481. Diaponible en: https://pubmed.ncbi.nlm.nih.gov/32105632/
6. Avilés Jurado FX, Prieto Alhambra D, González Sánchez N, De Ossó J, Arancibia C, Rojas Lechuga MJ, et al. Timing, complications, and safety of tracheotomy in critically ill patients with COVID-19. JAMA Otolaryngol Head Neck Surg [Internet]. 2020 [citado 26 May 2024]; 147(1):1–8. Disponible en: https://pubmed.ncbi.nlm.nih.gov/33034625/
7. Al Omari A, Al-Ashqar R, AlabdAlrhman R, Nuseir A, Allan H, Alzoubi F. Assessment of the harms and potential benefits of tracheostomy in COVID-19 patients: Narrative review of outcomes and recommendations. Am J Otolaryngol [Internet]. 2021 [citado 26 May 2024];42(4). Disponible en: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7914376/
8. Chiesa Estomba CM, Lechien JR, Calvo Henriquez C, Fakhry N, Karkos PD, Peer S, et al. Systematic review of international guidelines for tracheostomy in COVID-19 patients. Oral Oncol [Internet]. 2020 [citado 26 May 2024]; 108. Disponible en: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7274612/
9. Adly A, Youssef TA, El-Begermy MM, Younis HM. Timing of tracheostomy in patients with prolonged endotracheal intubation: a systematic review. Eur Arch Otorhinolaryngol [Internet]. 2018 [citado 26 May 2024]; 275(3):679-690. Disponible en: https://pubmed.ncbi.nlm.nih.gov/29255970/
10. Ferri E, Boscolo NF, Pedruzzi B, Campolieti G, Scotto F, Baratto F, et al. Indications and timing for tracheostomy in patients with SARS CoV2-related. EurArchOtorhinolaryngol [Internet]. 2020 [citado 26 May 2024]; 277(8):2403-2404. Disponible en: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7250256/
11. Goldstein C, Deisher D, Gorman E, Sheikh F, Sifri Z, Glass NE. Tracheostomy is safe in patients with prolonged intubation after coronavirus disease 2019 Infection. J Surg Res [Internet]. 2021 [citado 26 May 2024];266: 361-365. Disponible en: https://pubmed.ncbi.nlm.nih.gov/34087619/
12. Li M, Yiu Y, Merrill T, Yildiz V, De Silva B, Matrka L. Risk factors for post tracheostomy tracheal stenosis. Otolaryngol Head NeckSurg [Internet]. 2018 [citado 26 May 2024];159(4):698-704. Disponible en: https://pubmed.ncbi.nlm.nih.gov/30130451/
13. Altman KW, Ha TN, Dorai VK, Mankidy BJ, Zhu H. Tracheotomy timing and outcomes in the critically ill: complexity and opportunities for progress. Laryngoscope [Internet]. 2021 [citado 26 May 2024]; 131(2):282-287. Disponible en: https://pubmed.ncbi.nlm.nih.gov/32277707/
14. Battaglini D, Missale F, Schiavetti I, Filauro M, Iannuzzi F, Ascoli A, et al. Tracheostomy timing and outcome in severe COVID-19: The Wean Trach Multicenter Study. J Clin Med [Internet]. 2021 [citado 26 May 2024];10(12):2651. Disponible en: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC8235219/
15. Khammas AH, Dawood MR. Timing of tracheostomy in intensive care unit patients. Int Arch Otorhinolaryngol [Internet]. 2018 [citado 26 May 2024];22(4):437-442. Disponible en: https://pubmed.ncbi.nlm.nih.gov/30357027/
16. Myer CM, O'Connor DM, Cotton RT. Proposed grading system for subglottic stenosis based on endotracheal tube sizes. Ann Otol Rhinol Laryngol [Internet]. 1994 [citado 26 May 2024]; 103(4 Pt 1):319-23. Disponible en: https://pubmed.ncbi.nlm.nih.gov/8154776/
17. Gosling AF, Bose S, Gomez E, Parikh M, Cook C, Sarge T, et al. Perioperative considerations for tracheostomies in the era of COVID-19. Anesth Analg [Internet]. 2020 [citado 26 May 2024]; 131(2):378-386. Disponible en:
https://pubmed.ncbi.nlm.nih.gov/32459668/
18. Huang C, Wang Y, Li X, Ren L, Zhao J, Hu Y, et al. Clinical features of patients infected with 2019 novel coronavirus in Wuhan, China. Lancet [Internet]. 2020 [citado 26 May 2024]; 395(10223):497-506. Disponible en:
https://pubmed.ncbi.nlm.nih.gov/31986264/
19. Brodsky MB, Levy MJ, Jedlanek E, Pandian V, Blackford B, Price C et al. Laryngeal injury and upper airway symptoms after oral endotracheal intubation with mechanical ventilation during critical care: A systematic review. Crit Care Med [Internet]. 2018 [citado 26 May 2024]; 46(12):2010-2017. Disponibl en: https://pubmed.ncbi.nlm.nih.gov/30096101/
20. Mahmood K, Cheng GZ, Van Nostrand K, Shojaee S, Wayne MT, Abbott M et al. Tracheostomy for COVID-19 respiratory failure: multidisciplinary, multicenter data on timing, technique, and outcomes. Ann Surg [Internet]. 2021 [citado 26 May 2024]; 274(2):234-239. Disponible en: https://pubmed.ncbi.nlm.nih.gov/34029231/
21. Simonnet A, Chetboun M, Poissy J, Raverdy V, Noulette J, Duhamel A, et al. High prevalence of obesity in Severe Acute Respiratory Syndrome Coronavirus-2 (SARS-CoV-2) requiring invasive mechanical ventilation [Internet]. 2020 [citado 26 May 2024]; 28(7):1195-1199. Disponible en: https://pubmed.ncbi.nlm.nih.gov/32271993/
22. Livneh N, Mansour J, Kassif Lerner R, Feinmesser G, Alon E. Early vs. late tracheostomy in ventilated COVID-19 patients - A retrospective study. Am J Otolaryngol [Internet]. 2021 [citado 26 May 2024]; 42(6):103102. Disponible en: https://pubmed.ncbi.nlm.nih.gov/34120008/
23. Gowardman JR. Acute laryngeal injury following mechanical ventilation: revisiting the known unknowns. Crit Care Med [Internet]. 2019 [citado 26 May 2014]; 47(12):1802-1804. Disponible en: https://pubmed.ncbi.nlm.nih.gov/31738247/
24. Palacios JM, Bellido DA, Valdivia FB, Ampuero PA, Figueroa CF, Medina C et al. Tracheal stenosis as a complication of prolonged intubation in coronavirus disease 2019 (COVID-19) patients: a Peruvian cohort. J ThoracDis [Internet]. 2022 [citado 26 May 2024];14(4):995-1008. Disponible en: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC9096309/
25. París F, Borro JM, Tarrazona V, Casillas M, Galan G, Caffarena JM Jr et al. Management of non-tumoral tracheal stenosis in 112 patients. Eur J Cardiothorac Surg [Internet]. 1990 [citado 26 May 2024];4(5):265-8; Disponible en: https://pubmed.ncbi.nlm.nih.gov/2357392/
26. Lucchi M, Ambrogi M, Aprile V, Ribechini A, Fontanini G. Laryngotracheal resection for a post-tracheotomy stenosis in a patient with coronavirus disease 2019 (COVID-19). JTCVS Tech [Internet]. 2020 [citado 26 May 2024];4: 360-364. Disponiblelen:
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7423512/
27. Botti C, Lusetti F, Peroni S, Neri T, Castellucci A, Salsi P, et al. The role of tracheotomy and timing of weaning and decannulation in patients affected by severe COVID-19. Ear Nose Throat J[Internet]. 2021 [citado 26 May 2024];100(2suppl):116S-119S. Disponible en:
https://pubmed.ncbi.nlm.nih.gov/33035129/
28. Deng H, Fang Q, Chen K, Zhang X. Early versus late tracheotomy in ICU patients: A meta-analysis of randomized controlled trials. Medicine [Internet]. 2021 [citado 26 May 2024];100(3):e24329. Disponible en: https://pubmed.ncbi.nlm.nih.gov/33546065/
Published
Versions
- 2025-07-21 (2)
- 2024-09-24 (1)
How to Cite
Issue
Section
License
Copyright (c) 2025 Allan Fernando Arteaga-Hernández

This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License.
Copyright: Camagüey Medical Archive Magazine, offers immediately after being indexed in the SciELO Project; Open access to the full text of the articles under the principle of making available and free the research to promote the exchange of global knowledge and contribute to a greater extension, publication, evaluation and extensive use of the articles that can be used without purpose As long as reference is made to the primary source.
Conflicts of interest: authors must declare in a mandatory manner the presence or not of conflicts of interest in relation to the investigation presented.
(Download Statement of potential conflicts of interest)
The Revista Archivo Médico de Camagüey is under a License Creative Commons Attribution-Noncommercial-No Derivative Works 4.0 International (CC BY 4.0).
This license allows others to distribute, to mix, to adjust and to build from its work, even for commercial purposes, as long as it is recognized the authorship of the original creation. This is the most helpful license offered. Recommended for maximum dissemination and use of licensed materials. The full license can be found at: https://creativecommons.org/licenses/












 22 julio 2025
22 julio 2025