Evaluation of the state of frailty in older adults using the FRAIL scale
Abstract
Introduction: Population aging occurs in a heterogeneous manner, and this has profound implications for the planning and provision of health and social care, with frailty becoming a silent epidemic that affects older adults. This syndrome is potentially reversible with a multicomponent intervention. Primary health care is the preferred place for the diagnosis and monitoring of frailty, through scales such as the FRAIL scale.
Objective: To evaluate the state of frailty in a sample of older adults applying the FRAIL scale.
Methods: An observational, descriptive, cross-sectional study was carried out. The study universe consisted of 468 elderly people, where an intentional sample of 100 older adults was selected according to inclusion and exclusion criteria. The primary sources being observation and interview and as secondary sources the family health histories of the corresponding office, the individual medical records of each patient and a form that included the following variables: socio-demographic characteristics (age groups, sex), health conditions (comorbilities) and frailty status.
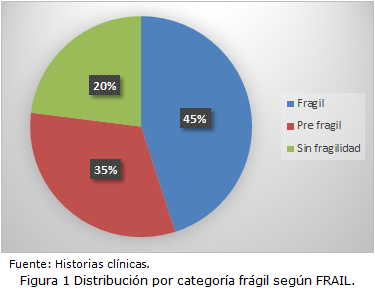
Results: The study was dominated by adults aged 70-79 years, female and with high blood pressure. The state of frailty was more frequent in 45% of the sample. A breakdown of the results is carried out according to sex, with the state of fragility predominating in women with 25% above the 20% obtained in men. Demonstrating the prevalence of the state of fragility in the selected sample, with a greater predisposition in the female population.
Conclusions: It is concluded that there is a greater frequency of frail older adults, so this study seeks to draw attention to the importance of evaluating frailty in all geriatric patients, in order to detect it in time and avoid the development of dependency and disability.
DeCS: FRAIL ELDERLY; FRAILTY; PRIMARY HEALTH CARE, OBSERVATIONAL STUDY; PREVALENCIA.
Downloads
References
1. Abreus-Mora J, González-Curbelo V. Fragilidad en adultos mayores y actividad física. Finlay [Internet]. 2023 [citado 11 Feb 2024];13(1):[aprox. 3 p.]. Disponible en: https://revfinlay.sld.cu/index.php/finlay/article/view/1235
2. Oficina Nacional de Estadística e Información de la República de Cuba. El envejecimiento de la población, Cuba y sus territorios 2021 [Internet]. Cuba: Centro de Estudio de Población y Desarrollo; 2022 [citado 10 Ago 2022]. Disponible en: http://www.onei.gob.cu/sites/default/files/el_envejecimiento_de_la_poblacion_de_cuba_y_sus_territorios_0.pdf
3. Casas HA, Cadore EL, Martínez N, Izquierdo M. El ejercicio físico en el anciano frágil: una actualización. Rev Esp Geriatr Gerontol [Internet]. 2015 [citado 11 Feb 2023];50(2):[aprox. 7p]. Disponible en: https://pesquisa.bvsalud.org/portal/resource/pt/ibc-134278
4. Vavasour G, Giggins OM, Doyle J, Daniel Kelly D. How wearable sensors have been utilised to evaluate frailty in older adults: a systematic review. J J Neuro Engineering Rehabil [Internet]. 2021 [citado 11 Feb 2023];18:112. Disponible en: https://jneuroengrehab.biomedcentral.com/articles/10.1186/s12984-021-00909-0
5. Bustos-Viviescas BJ, Alonso Acevedo-Mindiola A, Lozano Zapata RE. Grasa corporal y fuerza prensil de la mano: asociación por edades y sexos en sujetos aparentemente sanos. Rev cuban invest bioméd [Internet]. 2023 [citado 17 Feb 2023];42:e1264. Disponible en: https://revibiomedica.sld.cu/index.php/ibi/article/view/1264/1179
6. Ramos AM, Yordi M. Envejecimiento demográfico en Cuba y los desafíos que presenta para el Estado. Medwave [Internet]. Feb 2018 [citado 11 Feb 2023];18(4):[aprox. 10 p.]. Disponible en: https://www.medwave.cl/enfoques/ensayo/7231
7. Lauretani F, Ticinesi A, Gionti L, Prati B, Nouvenne A, Tana C. Short-Physical Performance Battery (SPPB) score is associated with falls in older outpatients. Aging Clin Exp Res [Internet]. 2019 [citado 11 Feb 2023];31(10):1435-42. Disponible en: https://doi.org/10.1007/s40520-018-1082-y
8. Acosta-Benito MA, Martín-Lesende I. Fragilidad en atención primaria: diagnóstico y manejo multidisciplinar. Atencion Primaria [Internet]. 2022 [citado 15 Feb 2023];54(2):9:[aprox. 5 p.]. Disponible en: https://dialnet.unirioja.es/servlet/articulo?codigo=8563619
9. García Quiñones R. Cuba: envejecimiento, dinámica familiar y cuidados. Noved poblac [Internet]. 2023 [citado 11 Feb 2024];15(29). Disponible en: https://revistas.uh.cu/novpob/article/view/574
10. Reeves D, Pye S, Ashcroft DM, Clegg A. The challenge of ageing populations and patient frailty: can primary care adapt? BMJ [Internet]. 2018 [citado 21 Feb 2023];362:k3349. Disponible en: http://dx.doi.org/10.1136/bmj.k3349
11. Camafort M, Kario K. Hypertension. heart failure, and frailty in older people: A common but unclear situation. J Clin Hypertens (Greenwich) [Internet]. 2020 [citado 21 Feb 2023];22:1763-8. Disponible en: http://dx.doi.org/10.1111/jch.14004
12. Assar ME, Laosa O, Portyuguéz L. Diabetes and frailty. Curr Opin Clin Nutr Metab Care [Internet]. 2019 [citado 21 Feb 2023];22:52-7. Disponible en: http://dx.doi.org/10.1097/MCO. 0000000000000535
13. Martin-Lesende I, Acosta-Benito MA, Goñi Ruiz N, Herreros-Herreros Y. Visión del manejo de la fragilidad en Atención Primaria. Rev Esp Salud Pública [Internet]. 2021 [citado 15 Feb 2023];95:e 2173-9110. Disponible en: https://dialnet.unirioja.es/servlet/articulo?codigo=8201232
14. Kojima G, Iliffe S, Walters K. Frailty index as a predictor of mortality: a systematic review and meta-analysis. Age Ageing [Internet]. 2018 [citado 15 Feb 2023];47:193-200:[aprox. 5 p]. Disponible en: http://dx.doi.org/10.1093/ageing/afx162
15. Coker JF, Martin ME, Simpson RM, Lafortune L. Frailty: an in-depth qualitative study exploring the views of community care staff. BMC Geriatr [Internet]. 2019 [citado 15 Feb 2023];19:47. Disponible en: http://dx.doi.org/10. 1186/s12877-019-1069-3
16. Segura-Cardona A, Cardona-Arango D. Mortalidad y años potenciales de vida perdidos por causas externas: Colombia 1998-2015. Univ Salud [Internet]. 2018 [citado 15 Feb 2023];20(2):149-59. Disponible en: http://dx.doi.org/10.22267/rus.182002.119
17. Li CY, Al Snih S, Karmarkar A, Markides KS, Ottenbacher KJ. Early frailty transition predicts 15-year mortality among nondisabled older Mexican Americans. Ann Epidemiol [Internet]. 2018 [citado 15 Feb 2023];28(6):362-67. Disponible en: https://doi.org/10.1016/j.annepidem.2018.03.021
18. Andrew MK, Dupuis-Blanchard S, Maxwell C, Giguere A, Keefe J, Rockwood K. Social and societal implications of frailty, including impact on Canadian healthcare systems. J Frailty Aging [Internet]. 2018 [citado 15 Feb 2023];7(4):217-23. Disponible en: https://doi.org/10.14283/jfa.2018.30
19. Junius-Walker U, Onder G, Soleymani D, Wiese B, Albaina O, Bernabei R, et al. The essence of frailty: a systematic review and qualitative synthesis on frailty concepts and definitions. Eur J Int Med [Internet]. 2018 [citado 15 Feb 2023];56:3-10. Disponible en: http://dx.doi.org/10.1016/j.ejim.2018.04.023
20. Oviedo-Briones M, Laso AR, Carnicero JA, Cesari M, Grodzicki T, Gryglewska B, et al. A Comparison of Frailty Assessment Instruments in Different Clinical and Social Care Settings: The Frail tools Project. J Am Med Dir Assoc [Internet]. 2021 [citado 21 Feb 2023];22(3). Disponible en: http://dx.doi.org/10.1016/j.jamda.2020.09.024
21. Ruiz JG, Dent E, Morley JE, Merchant RA, Beilby J, Beard J, et al. Screening for and Managing the Person with Frailty in Primary Care: ICFSR Consensus Guidelines. J Nutr Health Aging [Internet]. 2020 [citado 21 Feb 2023];24:920-7. Disponible en: http://dx.doi.org/10.1007/s12603-020-1492-3
22. Dolenc E, Rotar-Pavlic D. Frailty assessment scales for the elderly and their application in primary care: a systematic literature review. Zdr Varst [Internet]. 2019 [citado 21 Feb 2023];58:91-100. Disponible en: http://dx.doi.org/10.2478/sjph-2019-0012
23. Ambagtsheera RC, Beilbya JJ, Visvanathana R, Dent E, Yu S, Braunack-Mayer AJ. Should we screen for frailty in primary care settings? A fresh perspective on the frailty evidence base: A narrative review. Prev Med [Internet]. 2019 [citado 21 Feb 2023];19:63-9. Disponible en: http://dx.doi.org/10.1016/j.ypmed.2018.12.020
Published
How to Cite
Issue
Section
License
Copyright (c) 2024 Lázaro Davis-Varona

This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License.
Copyright: Camagüey Medical Archive Magazine, offers immediately after being indexed in the SciELO Project; Open access to the full text of the articles under the principle of making available and free the research to promote the exchange of global knowledge and contribute to a greater extension, publication, evaluation and extensive use of the articles that can be used without purpose As long as reference is made to the primary source.
Conflicts of interest: authors must declare in a mandatory manner the presence or not of conflicts of interest in relation to the investigation presented.
(Download Statement of potential conflicts of interest)
The Revista Archivo Médico de Camagüey is under a License Creative Commons Attribution-Noncommercial-No Derivative Works 4.0 International (CC BY 4.0).
This license allows others to distribute, to mix, to adjust and to build from its work, even for commercial purposes, as long as it is recognized the authorship of the original creation. This is the most helpful license offered. Recommended for maximum dissemination and use of licensed materials. The full license can be found at: https://creativecommons.org/licenses/












 22 julio 2025
22 julio 2025