Fracturas osteocondrales de la rodilla
Resumen
Introducción: Las fracturas osteocondrales que afectan la articulación de la rodilla se presenta de forma aislada o asociada a otras afecciones traumáticas. El diagnóstico inicial es en ocasiones difícil de realizar por la convergencia de signos clínicos e imagenológicos.
Objetivo: Brindar información actualizada sobre los elementos más importantes de esta enfermedad traumática.
Métodos: La búsqueda y el análisis de la información se realizó en un periodo de 31 días (del primero al 31 de agosto de 2021) y se emplearon las siguientes palabras del idioma ingles: osteochondral lesions, osteochondral fractures, osteochondral injuries a partir de la información obtenida se realizó una revisión bibliográfica de un total de 315 artículos publicados en las bases de datos PubMed, Hinari, SciELO y Medline mediante el gestor de búsqueda y administrador de referencias EndNote.
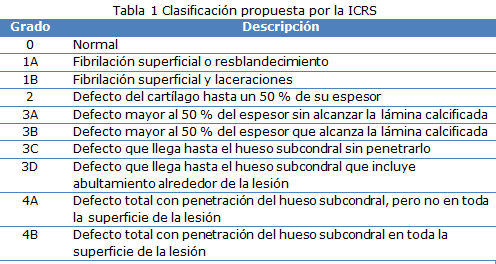
Resultados: Se hace referencia al mecanismo de producción, aspecto artroscópico, localización, características en cuanto a extensión, profundidad, clasificación y desplazamiento. Se describen las modalidades imagenológicas empleadas en el diagnóstico y su utilidad. Con relación al diagnóstico diferencial se describen un grupo de enfermedades con características similares. Se mencionan las modalidades de tratamiento basadas en el tamaño y tiempo de evolución.
Conclusiones: Las fracturas osteocondrales son lesiones frecuentes, para su diagnóstico se necesita de un alto índice de sospecha, ya que el diagnóstico clínico e imagenológico inicial no son concluyentes en la mayoría de los pacientes por estar combinada con otras afecciones.
DeCS: RODILLA; ARTROSCOPÍA/métodos; FRACTURAS ÓSEAS; CONDROCITOS; LITERATURA DE REVISIÓN COMO ASUNTO.
Descargas
Citas
1. Churchill JL, Krych AJ, Lemos MJ, Redd M, Bonner KF. A Case Series of Successful Repair of Articular Cartilage Fragments in the Knee. Am J Sports Med [Internet]. 2019 Sep [citado 25 Ene 2021];47(11):2589-95. Disponible en: https://pubmed.ncbi.nlm.nih.gov/31479328/
2. Dekker TJ, De Phillipo NN, Kennedy MI, Aman ZS, LaPrade RF. An Acute Osteochondral Defect Secondary to Fabella Impaction: A Case Report. JBJS Case Connect [Internet]. 2020 Oct-Dic [citado 30 Jul 2021];10(4):e2000513. Disponible en: https://pubmed.ncbi.nlm.nih.gov/34061479/
3. Chahla J, Stone J, Mandelbaum BR. How to manage cartilage injuries? Arthroscopy [Internet]. 2019 Oct [citado 30 Jul 2021]35(10):[aprox.2 p.]. Disponible en: https://www.arthroscopyjournal.org/article/S0749-8063(19)30721-2/fulltext
4. Kim D, Cho HH, Thangavelu M, Song C, Kim HS, Choi MJ, et al. Osteochondral and bone tissue engineering scaffold prepared from Gallus var domesticus derived demineralized bone powder combined with gellan gum for medical application. Int J Biol Macromol [Internet]. 2020 Apr [citado 30 Jul 2021];149:[aprox.3 p.]. Disponible en: https://pubmed.ncbi.nlm.nih.gov/31978480/
5. Zamborsky R, Danisovic L. Surgical Techniques for Knee Cartilage Repair: An Updated Large-Scale Systematic Review and Network Meta-analysis of Randomized Controlled Trials. Arthroscopy [Internet]. 2020 Mar [citado 25 Ene 2021];36(3):845-858. Disponible en: https://pubmed.ncbi.nlm.nih.gov/32139062/
6. Hacken BA, La Prade MD, Stuart MJ, Saris DBF, Camp CL, Krych AJ. Small cartilage defect management. J Knee Surg [Internet]. 2020 Dec [citado 25 Ene 2021];33(12): [aprox. 6 p.]. Disponible en: https://pubmed.ncbi.nlm.nih.gov/32898908/
7. Bronstein RD, Schaffer JC. Physical examination of the knee: meniscus, cartilage, and patellofemoral conditions. J Am Acad Orthop Surg [Internet]. 2017 May [citado 25 Ene 2021];25(5):[aprox.9 p.]. Disponible en: https://pubmed.ncbi.nlm.nih.gov/28406879/
8. Holz J, Spalding T, Boutefnouchet T, Emans P, Eriksson K, Brittberg M, et al. Patient-specific metal implants for focal chondral and osteochondral lesions in the knee; excellent clinical results at 2 years. Knee Surg Sports Traumatol Arthrosc [Internet]. 2021 [citado 30 Jul 2021];29(9):2899-2910. Disponible en: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC8384793/
9. Krych AJ, Saris DBF, Stuart MJ, Hacken B. Cartilage injury in the knee: assessment and treatment options. J Am Acad Orthop Surg [Internet] 2020 Nov [citado 30 Jul 2021];28(22):[aprox.8 p.]. Disponible en: https://pubmed.ncbi.nlm.nih.gov/32796370/
10. Nguyen JC, Green DW, Lin BF, Endo Y. Magnetic resonance evaluation of the pediatric knee after arthroscopic fixation of osteochondral lesions with biodegradable nails. Skeletal Radiol [Internet]. 2020 Ene [citado 25 Ene 2021];49(1):65-73. Disponible en: https://pubmed.ncbi.nlm.nih.gov/31214727/
11. Calcei JG, Ray T, Sherman SL, Farr J. Management of large focal chondral and osteochondral defects in the knee. J Knee Surg [Internet]. 2020 Dec [citado 30 Jul 2021];33(12):[aprox.3 p.]. Disponible en: https://pubmed.ncbi.nlm.nih.gov/33260221/
12. Gómez Cimiano FJ, Garcés Zarzalejo C, M de León LRE, Gómez de la Lastra L, Galindo Rubin C. Osteochondral allograft transplantation in the knee, after prolonged fresh storage at 37C. Determination of viability of human cartilage allografts, indications, technique, and evidence. Follow up 10 years. Rev Esp Cir Ortop Traumatol [Internet]. 2021 Sep-Oct [citado 30 Jul 2021];65(5):340-48. Disponible en: https://www.sciencedirect.com/science/article/pii/S1988885621000560
13. Jones KJ, Kelley BV, Arshi A, McAllister DR, Fabricant PD. Comparative Effectiveness of Cartilage Repair With Respect to the Minimal Clinically Important Difference. Am J Sports Med [Internet]. 2019 Nov [citado 30 Jul 2021];47(13):3284-93. Disponible en: https://pubmed.ncbi.nlm.nih.gov/31082325/
14. Mirzayan R, Charles MD, Batech M, Suh BD, DeWitt D. Bipolar Osteochondral Allograft Transplantation of the Patella and Trochlea. Cartilage [Internet]. 2020 Oct [citado 30 Jul 2021];11(4):431-40. Disponible en: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7488947/
15. Dwyer T, Theodoropoulos JS. Assessment of knee cartilage injury: Arthroscopic evaluation and classification. En: Gahunia HK, Gross AE, Pritzker KPH, Babyn PS, Murnaghan L, editors. Articular cartilage injury. Springer: Cham; 2020. p.215-231.
16. Lamplot JD, Schafer KA, Matava MJ. Treatment of Failed Articular Cartilage Reconstructive Procedures of the Knee: A Systematic Review. Orthop J Sports Med [Internet]. 2018 Mar [citado 30 Jul 2021];6(3):[aprox.6 p.]. Disponible en: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5871060/
17. Alosaimi MN, Almutairi MM, Alshahrani SM, Alqahtani MN, Alghamdi AS. Osteochondral fracture of the patella without soft tissue injury and with no dislocation: A case report. Int J Surg Case Rep [Internet]. 2021 Ene [citado 25 Ene 2021];78:48-53. Disponible en: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7736762/
18. Cinats D, Miller S, Abusara Z, Heard SM, Hutchison C, Schachar N, et al. Evolution of a Novel Tissue Preservation Protocol to Optimize Osteochondral Transplantation Outcomes. Cartilage [Internet]. 2021 Ene [citado 30 Jul 2021];12(1):31-41. Disponible en: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7755968/
19. Davey A, Frank RM, Wang KC, Southworth TM, Cole BJ. Clinical Outcomes of Revision Osteochondral Allograft Transplantation. Arthroscopy [Internet]. 2019 Sep [citado 25 Ene 2021];35(9):2636-2645. Disponible en: https://pubmed.ncbi.nlm.nih.gov/31500750/
20. Kizaki K, El-Khechen HA, Yamashita F, Duong A, Simunovic N, Musahl V, et al. Arthroscopic versus open osteochondral autograft transplantation (Mosaicplasty) for cartilage damage of the knee: a systematic review. J Knee Surg [Internet]. 2021 Jan [citado 30 Jul 2021];34(1):[aprox.13 p.]. Disponible en: https://pubmed.ncbi.nlm.nih.gov/31288271/
21. Megremis P, Megremis O, Margariti R. Late Repair, One Year After a Knee Twisting Injury, of a Missed Femoral Trochlea Osteochondral Fragment, With Bioabsorbable Nails, in a 14-Year-Old Boy. J Am Acad Orthop Surg Glob Res Rev [Internet]. 2019 Ago [citado 30 Jul 2021];3(8):e040. Disponible en: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6754220/
22. Cavendish PA, Everhart JS, Peters NJ, Sommerfeldt MF, Flanigan DC. Osteochondral allograft transplantation for knee cartilage and osteochondral defects: a review of indications, technique, rehabilitation, and outcomes. JBJS Rev [Internet]. 2019 Jun [citado 30 Jul 2021];7(6):e7. Disponible en: https://pubmed.ncbi.nlm.nih.gov/31220000/
23. Park SH, Yoo JH, Yoon HK, Chung K. Osteochondral Fracture of Posterior Aspect of Lateral Femoral Condyle After Lateral Patella Dislocation: A Case Report. JBJS Case Connect [Internet]. 2020 Ene-Mar [citado 30 Jul 2021];10(1):e1800366. Disponible en: https://pubmed.ncbi.nlm.nih.gov/32224666/
24. Penttilä P, Liukkonen J, Joukainen A, Virén T, Jurvelin JS, Töyräs J, et al. Diagnosis of Knee Osteochondral Lesions With Ultrasound Imaging. Arthrosc Tech [Internet]. 2015 Oct [citado 30 Jul 2021];4(5):e429-e433. Disponible en: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4662008/
25. Nimkingratana P, Brittberg M. Returning to Work After Articular Cartilage Repair Intervention: A Systematic Review. Orthop J Sports Med [Internet]. 2020 Mar [citado 25 Ene 2021];8(3):[aprox.3 p.]. Disponible en: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7074519/
26. Sheppard WL, Hinckel BB, Arshi A, Sherman SL, Jones KJ. Accurate Reporting of Concomitant Procedures is Highly Variable in Studies Investigating Knee Cartilage Restoration. Cartilage [Internet]. 2021 Jul [citado 25 Ene 2021];12(3):333-343. Disponible en: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC8236649/
27. Riboh JC, Cvetanovich GL, Cole BJ, Yanke AB. Comparative efficacy of cartilage repair procedures in the knee: a network meta-analysis. Knee Surg Sports Traumatol Arthrosc [Internet]. 2017 Dic [citado 30 Jul 2021];25(12):3786-99. Disponible en: https://pubmed.ncbi.nlm.nih.gov/27605128/
28. Gorbachova T, Melenevsky Y, Cohen M, Cerniglia BW. Osteochondral lesions of the knee: differentiating the most common entities at MRI. Radiographics [Internet]. 2018 Sep-Oct [citado 30 Jul 2021];38(5):[aprox.8 p.]. Disponible en: https://pubmed.ncbi.nlm.nih.gov/30118392/
29. Nie X, Yang J, Chuah YJ, Zhu W, Peck Y, He P, et al. Full-scale osteochondral regeneration by sole graft of tissue-engineered hyaline cartilage without co-engraftment of subchondral bone substitute. Adv Healthc Mater [Internet]. 2020 Jan [Citado 25 Ene 2021];9(2):[aprox.3 p.]. Disponible en: https://pubmed.ncbi.nlm.nih.gov/31820592/
30. Ogura T, Ackermann J, Mestriner AB, Merkely G, Gomoll AH. The Minimal Clinically Important Difference and Substantial Clinical Benefit in the Patient-Reported Outcome Measures of Patients Undergoing Osteochondral Allograft Transplantation in the Knee. Cartilage [Internet]. 2021 Ene [citado 25 Ene 2021];12(1):42-50. Disponible en: https://pubmed.ncbi.nlm.nih.gov/30463426/
31. Inderhaug E, Solheim E. Osteochondral Autograft Transplant (Mosaicplasty) for Knee Articular Cartilage Defects. JBJS Essent Surg Tech [Internet]. 2019 Oct-Dic [citado 30 Jul 2021];9(4):e34. Disponible en: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6974309/
32. Skelley NW, Kurtenbach C, Kimber K, Piatt B, Noonan B. Return-to-sport review for current cartilage treatments. J Knee Surg [Internet]. 2021 Jan [citado 25 Ene 2021];34(1):[aprox.7 p.]. Disponible en: https://pubmed.ncbi.nlm.nih.gov/33389739/
33. Carey JL, Shea KG, Lindahl A, Vasiliadis HS, Lindahl C, Peterson L. Autologous Chondrocyte Implantation as Treatment for Unsalvageable Osteochondritis Dissecans: 10- to 25-Year Follow-up. Am J Sports Med [Internet]. 2020 Abr [citado 30 Jul 2021]; 48(5):1134-40. Disponible en: https://pubmed.ncbi.nlm.nih.gov/32181674/
34. Le H, Xu W, Zhuang X, Chang F, Wang Y, Ding J. Mesenchymal stem cells for cartilage regeneration. J Tissue Eng [Internet]. 2020 Ene-Dic [citado 30 Jul 2021];11. Disponible en: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7457700/
35. Neri T, Dehon M, Klasan A, Putnis SE, Farizon F, Philippot R. Predictors of Functional Outcome After Microfracture Treatment of Cartilage Defects of the Knee. Surg Technol Int [Internet]. 2020 Nov [citado 30 Jul 2021];37:341-47. Disponible en: https://europepmc.org/article/med/33197956
36. Peñalver JM, Villalba J, Yela-Verdú CP, Sánchez J, Balaguer-Castro M. All-Arthroscopic Nanofractured Autologous Matrix-Induced Chondrogenesis (A-NAMIC) Technique for the Treatment of Focal Chondral Lesions of the Knee. Arthrosc Tech [Internet]. 2020 Jun [citado 30 Jul 2021];9(6):e755-759. Disponible en: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7301272/
37. Lychagin A, Lipina M, Garkavi A, Islaieh O, Timashev P, Ashmore K, et al. Intraosseous injections of platelet rich plasma for knee bone marrow lesions treatment: one year follow-up. Int Orthop [Internet]. 2020 Mar [citado 30 Jul 2021]. Disponible en: https://orthoregen.ru/files/intraosseous_injections.pdf
38. Riff AJ, Huddleston HP, Cole BJ, Yanke AB. Autologous Chondrocyte Implantation and Osteochondral Allograft Transplantation Render Comparable Outcomes in the Setting of Failed Marrow Stimulation. Am J Sports Med [Internet]. 2020 Mar [citado 25 Ene 2021];48(4):861-70. Disponible en: https://pubmed.ncbi.nlm.nih.gov/32053398/
39. Tauro TM, Gifford A, Haunschild ED, Gilat R, Fu MC, Cole BJ. Cartilage Restoration Using Dehydrated Allogeneic Cartilage, Platelet-Rich Plasma, and Autologous Cartilage Mixture Sealed With Activated Autologous Serum. Arthrosc Tech [Internet]. 2020 Jun [citado 30 Jul 2021];9(6):e847-e857. Disponible en: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7301379/
40. Sharafat-Vaziri A, Khorasani S, Darzi M, Saffarian Z, Alizadeh Z, Tahmasebi MN, et al. Safety and efficacy of engineered tissue composed of silk fibroin/collagen and autologous chondrocytes in two patients with cartilage defects: A pilot clinical trial study. Knee. 2020 Oct [citado 30 Jul 2021];27(5):[aprox.9 p.]. Disponible en: https://linkinghub.elsevier.com/retrieve/pii/S0968-0160(20)30168-X
41. Li ZX, Song HH, Wang Q, Guo DM. Clinical outcomes after absorbable suture fixation of patellar osteocondral fracture following patellar dislocation. Ann Transl Med [Internet]. 2019 Abr [citado 30 Jul 2021];7(8):173. Disponible en: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6526275/
42. Schuette HB, Kraeutler MJ, Schrock JB, McCarty EC. Primary Autologous Chondrocyte Implantation of the Knee Versus autologous Chondrocyte Implantation After Failed Marrow Stimulation: A Systematic Review. Am J Sports Med [Internet]. 2020 [citado 25 Ene 2021];49(9). Disponible en: https://journals.sagepub.com/doi/abs/10.1177/0363546520968284
43. Yanke AB, Lee AS, Karas V, Abrams G, Riccio ML, Verma NN, et al. Surgeon Ability to Appropriately Address the Calcified Cartilage Layer: An In Vitro Study of Arthroscopic and Open Techniques. Am J Sports Med [Internet]. 2019 Sep [citado 25 Ene 2021];47(11):2584-88. Disponible en: https://pubmed.ncbi.nlm.nih.gov/31336053/
44. Schlechter JA, Nguyen SV, Fletcher KL. Utility of Bioabsorbable Fixation of Osteochondral Lesions in the Adolescent Knee: Outcomes Analysis With Minimum 2-Year Follow-up. Orthop J Sports Med [Internet]. 2019 Oct [citado 25 Ene 2021];7(10). Disponible en: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6820181/
45. Zhou S, Cai M, Huang K. Treatment of osteochondral fracture of the lateral femoral condyle with TWINFIX Ti suture anchor X-shaped internal fixation under arthroscopy: a surgical technique and three cases report. Orthop Surg [Internet]. 2020 Apr [citado 25 Ene 2021];12(2):[aprox.6 p.]. Disponible en: https://pubmed.ncbi.nlm.nih.gov/32162472/
46. Samitier G, Vinagre G, Cugat R, Seijas R, Barastegui D. One-Stage Osteochondral Fracture Repair Technique With knotless Anchors and Internconnected Crossing Suture Sliding Loops for the Knee. Arthrosc Tech [Internet]. 2020 Nov [citado 25 Ene 2021];9(11):e1813-e1818. Disponible en: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7695622/
47. Stannard JP, Stannard JT, Schreiner AJ. Fresh Osteochondral allograft transplants in the knee: bipolar and beyond. Knee Surg [Internet]. 2020 Dec [citado 30 Jul 2021];33(12):[aprox.7 p.]. Disponible en: https://pubmed.ncbi.nlm.nih.gov/32688399/
48. Temple HT. Allograft reconstruction of the knee-methods and outcomes. J Knee Surg [Internet]. 2019 Apr [citado 30 Jul 2021];32(4):[aprox.6 p.]. Disponible en: https://pubmed.ncbi.nlm.nih.gov/30261530/
Publicado
Cómo citar
Número
Sección
Licencia
La Revista Archivo Medico Camagüey, ofrece de forma inmediata después de ser indexada en el Proyecto SciELO; acceso abierto al texto completo de los artículos bajo el principio de hacer disponible y gratuita la investigación para favorecer el intercambio del conocimiento global y coadyuvar a una mayor extensión, publicación, evaluación y uso extensivo de los artículos que se exponen pudiendo ser utilizados, sin fines comerciales, siempre y cuando se haga referencia a la fuente primaria.
Carta De Declaración De Autoría u Derechos De Autor(a)
Conflictos de intereses: los autores deberán declarar de forma obligatoria la presencia o no de conflictos de intereses en relación con la investigación presentada. (Descargar Plantilla para declarar confictos de intereses)
La Revista Archivo Médico Camagüey se encuentra bajo una
Licencia Creative Commons Reconocimiento-NoComercial 4.0 International (CC BY NC 4.0).
Esta licencia permite a otros distribuir, mezclar, ajustar y construir a partir de su obra, incluso con fines comerciales, siempre que le sea reconocida la autoría de la creación original. Esta es la licencia más servicial de las ofrecidas. Recomendada para una máxima difusión y utilización de los materiales sujetos a la licencia. La licencia completa puede consultarse en: https://creativecommons.org/licenses/












